The Hidden Dangers of Common Prescriptions
Benzodiazepine addiction therapy is a specialized treatment approach that combines medically supervised detox, behavioral therapies like CBT, and ongoing support to help individuals safely withdraw from benzodiazepines and build lasting recovery. Treatment typically includes:
- Medical detox with gradual tapering to prevent dangerous withdrawal symptoms like seizures
- Cognitive-Behavioral Therapy (CBT) to identify triggers and develop healthy coping skills
- Support groups like Narcotics Anonymous for peer connection and accountability
- Individualized treatment plans addressing co-occurring mental health disorders
- Family involvement through education and therapy to strengthen recovery support
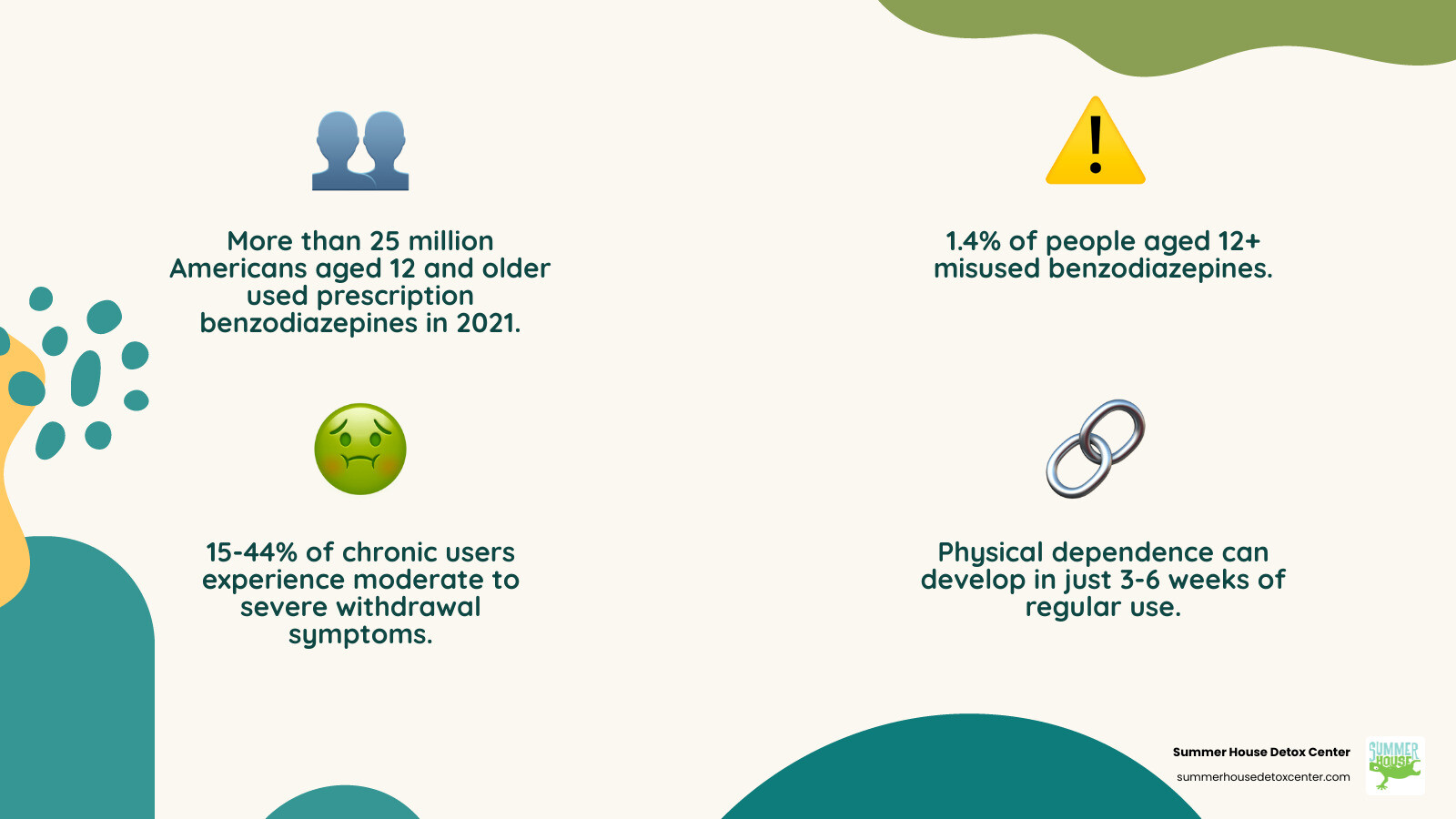
If you’ve been prescribed Xanax, Valium, Ativan, or Klonopin for anxiety or insomnia, you’re not alone. In 2021, more than 25 million Americans aged 12 and older used prescription benzodiazepines. These medications work effectively for short-term relief, but they carry a hidden danger most people don’t expect.
What starts as legitimate medical treatment can quickly spiral into dependence. Research shows that just 3 to 6 weeks of regular use can lead to physical dependence, even at prescribed doses. Between 15-44% of chronic benzodiazepine users experience moderate to severe withdrawal symptoms when they try to stop.
Here in Miami and throughout Florida, many people find themselves trapped by medications their doctors prescribed to help them. You might recognize yourself in this story: you started taking benzos as directed, but now you need higher doses to feel the same relief. Maybe you’ve tried to quit on your own but faced terrifying withdrawal symptoms. Perhaps you feel ashamed, wondering how a prescription turned into a problem you can’t control alone.
You haven’t failed. Benzodiazepines are simply more powerful than most people realize. The good news? Recovery is absolutely possible with the right support and treatment approach.
The Slippery Slope: From Prescription to Dependence
Benzodiazepines, often referred to simply as “benzos,” are a class of sedative medications widely prescribed for various conditions. They include well-known names like Xanax (alprazolam), Valium (diazepam), Ativan (lorazepam), and Klonopin (clonazepam). These medications are typically prescribed for their calming effects, which can be incredibly helpful for managing anxiety disorders, panic attacks, insomnia, muscle spasms, and certain types of seizures. They are also frequently used in medical settings for acute alcohol withdrawal management, a testament to their potent sedative properties.
So, how do these powerful medications work their magic in our brains? Benzodiazepines primarily function by enhancing the effects of gamma-aminobutyric acid (GABA), which is the main inhibitory neurotransmitter in the central nervous system. Think of GABA as your brain’s “brake pedal.” When benzodiazepines bind to specific sites on the GABA-A receptor complex, they essentially make this brake pedal more effective, slowing down brain activity. This results in the calming, anxiolytic (anxiety-reducing), hypnotic (sleep-inducing), and muscle-relaxant effects that make them so appealing for short-term relief.
While effective for short-term use, the very mechanism that makes benzodiazepines so powerful also contributes to their significant risks, particularly with long-term use. The brain quickly adapts to their presence, leading to physiological changes that can result in dependence and addiction. The harms from prolonged benzodiazepine use are well-recognized and include not only dependency but also cognitive decline, memory problems, and an increased risk of falls, especially in older adults.
It’s crucial to understand the distinction between physical dependence and a substance use disorder (addiction). Physical dependence means your body has adapted to the drug and will experience withdrawal symptoms if you stop using it. Almost everyone who takes benzodiazepines regularly for more than a month will develop some level of physical dependence. However, a substance use disorder is a more complex condition characterized by compulsive drug-seeking and use despite harmful consequences, and it occurs in less than 2% of people taking these medications. Unfortunately, the line between dependence and addiction can blur, and for many, dependence can pave the way for addiction. To learn more about the potential dangers, explore The Dark Side of Benzos.
Recognizing the Signs of Benzodiazepine Addiction
Identifying benzodiazepine addiction can be challenging, as it often begins with a legitimate prescription. However, certain signs and symptoms can indicate that use has crossed into misuse or addiction. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a diagnosis of a sedative, hypnotic, or anxiolytic use disorder requires at least two of the following symptoms to occur within a one-year period:
- Taking higher doses or using longer than intended: You might find yourself needing more of the medication to achieve the same calming effect, or using it for a longer duration than your doctor prescribed.
- Persistent desire or unsuccessful attempts to cut down or control use: You want to stop or reduce your intake but find yourself unable to, despite your best efforts.
- Spending excessive time obtaining, using, or recovering from the drug: Your life might start revolving around getting and taking the medication.
- Cravings: Experiencing an intense urge or desire for benzodiazepines.
- Neglecting responsibilities: Failing to fulfill obligations at work, school, or home due to drug use.
- Continued use despite negative consequences: You keep using benzos even when they cause or worsen physical, psychological, or social problems.
- Reduced recreational, social, or occupational activities: You lose interest in hobbies or social interactions you once enjoyed.
- Using in physically hazardous situations: For example, driving under the influence of benzodiazepines.
- Tolerance: Needing markedly increased amounts of the drug to achieve intoxication or the desired effect.
- Withdrawal symptoms or using to avoid them: Experiencing uncomfortable or severe physical and psychological symptoms when the drug wears off, and taking more to alleviate them.
Other observable signs might include loss of coordination, slurred speech, drowsiness or lethargy, slow reflexes, dizziness, changes in appetite, irritability, mood swings, confusion, or memory loss. In some cases, individuals may engage in “doctor shopping,” visiting multiple doctors to obtain prescriptions, which is a clear red flag. If you or a loved one in Florida exhibits these signs, it’s a strong indicator that professional help is needed.
The Critical First Step: Medically Supervised Benzodiazepine Detox
Once dependence or addiction to benzodiazepines has developed, the first critical step toward recovery is detoxification. This is a process that should never be attempted alone, especially with benzodiazepines, due to the potentially dangerous and even life-threatening nature of withdrawal.
What are the symptoms of benzodiazepine withdrawal, and why is medical supervision important during this process?
When someone who is physically dependent on benzodiazepines suddenly stops taking them or significantly reduces their dose, their brain, accustomed to the drug’s presence, reacts strongly to its absence. This leads to a range of withdrawal symptoms, often referred to as Benzodiazepine Withdrawal Syndrome. These symptoms can begin as early as a few hours after the last dose, depending on the half-life of the specific benzo.
Common withdrawal symptoms include:
- Severe anxiety and panic attacks
- Insomnia and other sleep disturbances
- Irritability and extreme mood swings
- Sweating and tremors
- Muscle pain and stiffness
- Nausea, vomiting, and other gastrointestinal issues
- Agitation and restlessness
- Hallucinations (visual, auditory, or tactile)
- Severe cravings for the drug
- Racing pulse and increased blood pressure
- Increased body temperature
- Overactive reflexes
- In severe cases, seizures and delirium
The risk of life-threatening complications, particularly seizures, is why medical supervision is not just recommended but absolutely essential during benzodiazepine withdrawal. Abrupt cessation after even a few weeks of use can trigger these severe events. Here at Summer House Detox Center in Miami, our team understands these risks intimately. We provide a safe, controlled environment where medical professionals can monitor your vital signs, manage symptoms, and intervene if complications arise. This medically supervised detox process is the cornerstone of safe withdrawal and the first step on your path to freedom. Learn more about our approach to Benzo Detox.
Managing Withdrawal Symptoms Safely
Managing benzodiazepine withdrawal is a delicate process that prioritizes safety and comfort. Instead of an abrupt stop, which is dangerous, the standard approach involves a gradual reduction of the medication.
What are the different approaches to managing benzodiazepine withdrawal?
The primary method is gradual tapering, where the dosage of the benzodiazepine is slowly decreased over time. This allows the brain and body to adjust to progressively lower amounts of the drug, minimizing the severity of withdrawal symptoms and reducing the risk of complications like seizures. The pace of tapering is highly individualized, depending on factors such as the type of benzodiazepine used, the dosage, the duration of use, and the individual’s overall health. A typical taper might last anywhere from eight weeks to four months, though for long-term users, it can extend to a year or even longer.
Another common strategy is substitution tapering. If a person is taking a short-acting benzodiazepine (like Xanax or Ativan), they may be switched to a longer-acting benzodiazepine, such as diazepam (Valium). Diazepam is often preferred because its longer half-life means it stays in the body for a longer period, resulting in more stable blood levels and less intense peaks and troughs, which can make the tapering process smoother and more manageable. Once stabilized on the longer-acting drug, the gradual reduction of the dosage begins.
Throughout this process, our medical team at Summer House Detox Center focuses on symptom management. We address acute withdrawal symptoms like anxiety, insomnia, muscle pain, and gastrointestinal issues (which can be particularly uncomfortable – for more on this, read Why Do I Experience Stomach and Digestive Problems When Quitting Benzos?). While there isn’t a single “magic bullet” medication to completely eliminate withdrawal discomfort, our team uses supportive care and, in some cases, adjunctive medications (which we’ll discuss further in the FAQ section) to help alleviate distress. Our goal is to make the withdrawal process as comfortable and safe as possible, setting the stage for successful long-term recovery. For insights into the duration of this process, see How Long Does Benzo Withdrawal Last?.
Comprehensive Benzodiazepine Addiction Therapy: Building a Foundation for Recovery
Completing medical detoxification is a monumental achievement, but it’s just the first chapter in the recovery journey. Detox addresses the physical dependence, safely removing the drug from the body. However, as our research indicates, detox alone “may not be able to fully address the behavioral, psychological, and social issues associated with addiction.” This is where comprehensive benzodiazepine addiction therapy comes in, building a robust foundation for lasting change.
After detox, individuals transition into a more intensive treatment phase. At Summer House Detox Center, we offer custom programs, including inpatient options, designed to address the unique needs of each person. Inpatient treatment provides a structured, supportive environment away from triggers and distractions, allowing for deep engagement in therapy. These programs are essential for exploring the root causes of addiction, developing coping mechanisms, and healing.
A crucial aspect of our approach is developing individualized treatment plans. We understand that addiction is a complex disease, often intertwined with co-occurring mental health disorders like depression, anxiety, or trauma. Our expert team works to identify and address these underlying issues simultaneously, as treating only the addiction without addressing co-occurring conditions can undermine long-term recovery. This holistic, personalized care is a hallmark of our programs here in Miami, recognizing that true healing means treating the whole person. To learn more about how we support this journey, visit Benzo Addiction Recovery.
Behavioral Therapies for Lasting Change
Behavioral therapies are the bedrock of effective benzodiazepine addiction therapy, equipping individuals with the tools and strategies needed to maintain sobriety and build a fulfilling life.
What are the various therapeutic interventions for benzodiazepine addiction?
Among the most effective is Cognitive-Behavioral Therapy (CBT). CBT helps individuals identify the thoughts, feelings, and behaviors that contribute to their benzodiazepine use. For example, someone might learn to recognize how stress or certain social situations trigger cravings, and then develop healthier coping skills to manage these triggers without resorting to medication. CBT challenges negative thought patterns and helps individuals develop more adaptive responses to life’s challenges.
Other valuable behavioral therapies include:
- Motivational Improvement Therapy (MET): This approach helps individuals resolve ambivalence about treatment and recovery, strengthening their motivation to change. It’s particularly useful in the early stages of therapy.
- Contingency Management (CM): CM uses positive reinforcement, such as vouchers or small rewards, for desired behaviors like negative drug tests. This incentivizes sobriety and can be very effective in promoting initial engagement and sustained abstinence.
The overarching role of psychotherapy in benzodiazepine addiction therapy is vital. It provides a safe space to process emotions, address unresolved trauma, and learn new ways of navigating life. These therapies empower individuals to understand why they used benzodiazepines beyond physical dependence and to develop sustainable strategies for long-term well-being.
The Power of Community: Support Groups and Family Involvement
No one should walk the path of recovery alone. The power of community and the involvement of loved ones are integral components of successful benzodiazepine addiction therapy.
How can family and loved ones support someone struggling with benzodiazepine addiction?
Support groups play a crucial role in providing a sense of community and shared understanding. Groups like Narcotics Anonymous (NA) offer a welcoming space where individuals can share their personal experiences, struggles, and triumphs with others who truly understand. This peer support can reduce feelings of isolation and shame, fostering connection and accountability. Hearing stories of recovery and overcoming similar challenges can be incredibly motivating and provide practical insights into maintaining sobriety.
Beyond peer support, the involvement of family and loved ones is profoundly impactful. Here’s how they can help:
- Educate themselves: Understanding the nature of benzodiazepine dependence and addiction, the withdrawal process, and the journey of recovery helps family members respond with empathy and knowledge.
- Encourage treatment: Supporting and encouraging a loved one to seek and commit to professional treatment is paramount.
- Be patient and understanding: Recovery is not linear. There will be good days and challenging days, and a loved one’s patience and unwavering support are invaluable.
- Establish healthy boundaries: This is crucial for both the individual in recovery and their family. Boundaries protect everyone’s well-being and prevent enabling behaviors.
- Seek support for themselves: Addiction affects the entire family system. Family therapy and support groups specifically for family members (like Al-Anon or Nar-Anon) can provide a safe space for loved ones to process their own emotions and learn healthy coping strategies.
At Summer House Detox Center in Miami, we believe in a holistic approach that often includes family education and therapy, recognizing that a supportive home environment is a powerful asset in long-term recovery.
Frequently Asked Questions about Benzodiazepine Treatment in Florida
We understand that you likely have many questions about benzodiazepine addiction therapy and treatment options, especially when seeking help in Florida. Here, we address some common concerns.
Can you overdose on benzodiazepines?
Yes, you absolutely can overdose on benzodiazepines. While an overdose of benzos alone may not always be fatal, the risk dramatically increases when combined with other substances, particularly central nervous system (CNS) depressants like opioids and alcohol. This polysubstance use is incredibly dangerous and is a leading cause of overdose deaths.
The signs of a benzodiazepine overdose include:
- Extreme drowsiness and lethargy
- Confusion or impaired mental status
- Slurred speech
- Impaired coordination and unsteadiness
- Slowed or shallow breathing (respiratory depression)
- Significantly decreased blood pressure
- Loss of consciousness or coma
When benzodiazepines are mixed with opioids or alcohol, their sedative effects are amplified, leading to severe respiratory depression that can stop breathing and result in death. It’s a critical danger, and unfortunately, we see the tragic consequences of polysubstance use here in Florida. If you or a loved one is struggling with this dangerous combination, please read What Happens If I Drink Alcohol While Using Benzos? for more information. Always call 911 immediately if you suspect an overdose.
What medications are used in benzodiazepine addiction therapy?
Pharmacotherapy plays a specific and crucial role in benzodiazepine addiction therapy, particularly during the detoxification and withdrawal phase. The primary goal is to manage withdrawal symptoms safely and prevent life-threatening complications.
- Diazepam: This long-acting benzodiazepine is often the single agent of choice for withdrawal management. As mentioned earlier, it’s used for gradual tapering or to substitute shorter-acting benzos, allowing for a smoother, more controlled reduction in dosage.
- Anticonvulsants: Medications like carbamazepine and pregabalin have shown some efficacy in reducing the severity of benzodiazepine withdrawal symptoms, particularly anxiety and seizure risk. They can help stabilize brain activity during the tapering process.
- Flumazenil: This medication acts as a benzodiazepine receptor antagonist. While not widely used for routine withdrawal due to its short half-life and potential to precipitate acute, severe withdrawal (including seizures) if administered too quickly or in high doses, it has been explored in specialized inpatient settings for rapid withdrawal under strict medical supervision. Its use is complex and carries significant risks, requiring expert clinical judgment.
While these medications aid in the physical withdrawal, they are not a cure for addiction itself. They are tools used to facilitate a safe detox, which must then be followed by comprehensive behavioral therapies and ongoing support to address the psychological aspects of addiction.
How do I find help for Xanax addiction in Miami?
If you or someone you care about is struggling with Xanax addiction in Miami or anywhere in Florida, finding the right help is a critical step towards recovery. Xanax (alprazolam) is a particularly potent and fast-acting benzodiazepine, making its withdrawal especially challenging and dangerous.
At Summer House Detox Center in Miami, we specialize in providing personalized, medically supervised detox services specifically for benzodiazepine addiction, including Xanax. Our experienced team, some of whom are in recovery themselves, understands the unique challenges of Xanax withdrawal and is dedicated to offering comfort, dignity, and unwavering support throughout the process. We create a safe environment where you can safely steer withdrawal symptoms under constant medical care, mitigating risks like seizures.
Finding local resources for benzodiazepine addiction therapy means looking for facilities that offer:
- Medically supervised detox: Essential for safe Xanax withdrawal.
- Individualized treatment plans: Custom to your specific needs, history, and co-occurring conditions.
- Comprehensive therapy: Including CBT and other behavioral interventions to address the psychological roots of addiction.
- Aftercare planning: Support to ensure sustained recovery once detox is complete.
- A supportive environment: One that promotes healing and fosters a sense of community.
We are proud to offer these services right here in Miami, FL. If you’re ready to take the first step towards breaking free from Xanax addiction, we are here to guide you. Learn more about our approach to Xanax Addiction Withdrawal Treatment and how you can Beat Xanax Addiction at Summer House Detox Center in Miami.
Conclusion: Start Your Recovery Journey in Miami Today
The journey to overcome benzodiazepine addiction might seem daunting, but we want you to know that recovery is not just a possibility—it’s a reality we help people achieve every day. Here at Summer House Detox Center in Miami, we understand the complexities of benzodiazepine dependence and addiction. We’ve seen how these medications, initially prescribed to help, can lead individuals down an unexpected path.
Our approach to benzodiazepine addiction therapy is built on the understanding that a multi-faceted strategy is key to success. It begins with safe, medically supervised detoxification, ensuring your physical well-being during the critical withdrawal phase. This crucial first step is then seamlessly integrated into a broader, long-term treatment plan that addresses the psychological, emotional, and social dimensions of addiction.
Long-term treatment plans and aftercare options are crucial for ensuring a sustainable and lasting recovery. They are designed to support you not only through the immediate challenges but also through the ongoing requirements of navigating life in sobriety. This includes continued engagement in behavioral therapies like CBT, participation in support groups, and the development of healthy coping skills to prevent relapse.
We believe in the importance of professional help, delivered with compassion and expertise. Our team at Summer House Detox Center is dedicated to providing personalized care, focusing on your comfort, dignity, and individual needs. We are here to offer a supportive hand, guiding you through every stage of your recovery journey in the vibrant, healing environment of Miami, Florida.
Don’t let benzodiazepine addiction define your future. You deserve a life free from dependence, filled with hope and genuine well-being. Take the first courageous step towards reclaiming your life. Contact us today and Find expert benzo detox services in Florida. We are ready to help you begin your path to freedom.