The Unseen Impact of the Opioid Crisis on Newborns
The opioid crisis has cast a long, devastating shadow across the United States, and its most innocent victims are often the most overlooked: newborns. When a pregnant person uses opioids, whether prescribed or illicit, the substance crosses the placenta and affects the developing baby. After birth, this supply is abruptly cut off, forcing the infant’s body into a state of withdrawal. This condition, known as Neonatal Abstinence Syndrome (NAS) or, more specifically, Neonatal Opioid Withdrawal Syndrome (NOWS), is a heart-wrenching reality for thousands of families each year.
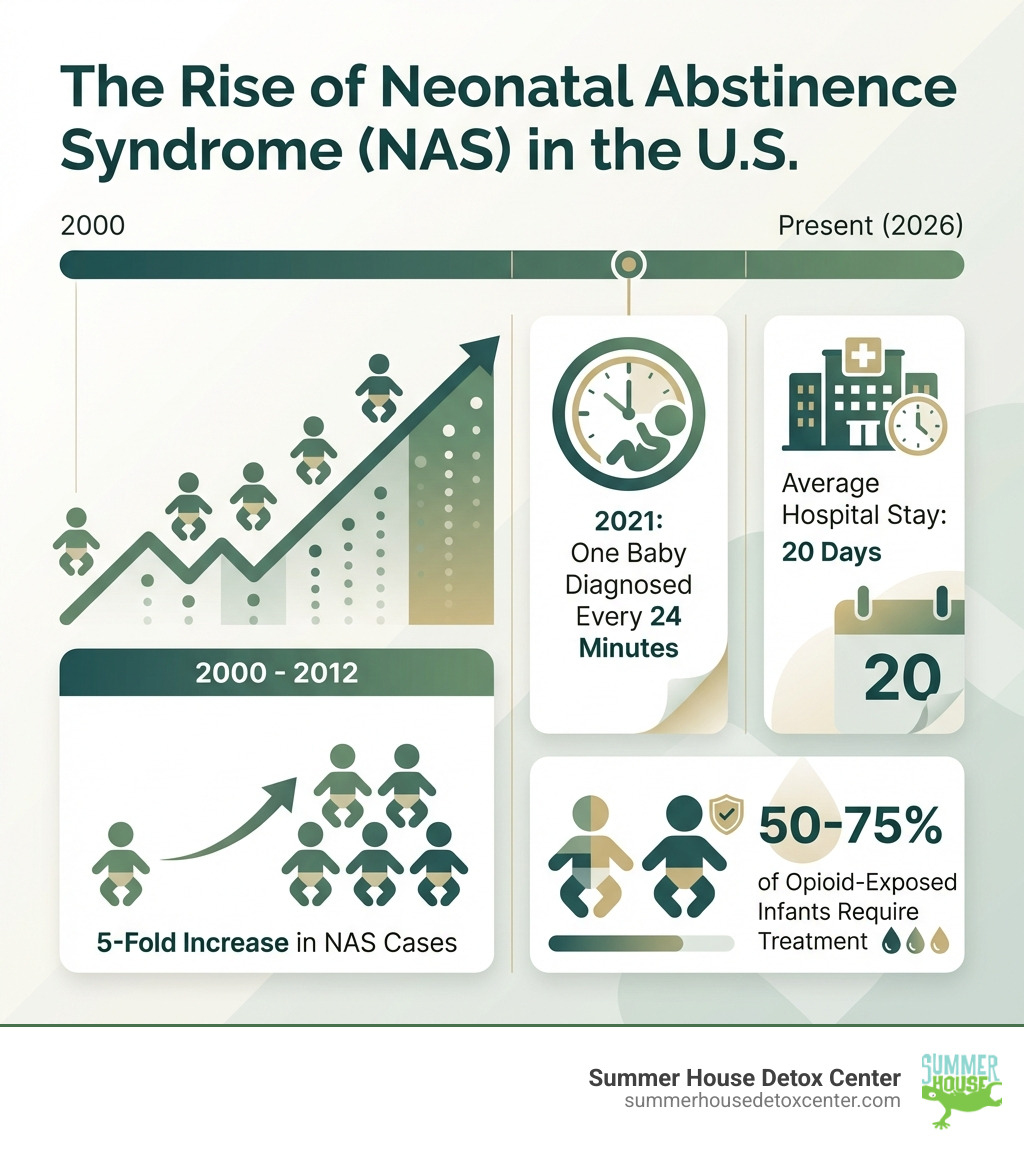
According to 2021 estimates, one baby is diagnosed with NAS every 24 minutes in the U.S.—that’s more than 59 newborns every single day. Here in Florida, we are not immune to this crisis. Communities from Miami to Jacksonville are seeing the direct impact of opioid use on their youngest and most vulnerable members. The rise in prescription opioid misuse, along with the prevalence of illicit substances like heroin and fentanyl, has led to a corresponding increase in the number of infants starting their lives in withdrawal. This places an immense emotional and financial burden on families and healthcare systems alike.
What are the main infant opiate withdrawal symptoms?
- High-pitched or excessive crying that’s hard to soothe
- Tremors or body shakes (often in the hands, arms, or legs)
- Feeding difficulties including poor sucking, vomiting, or refusing to eat
- Sleep problems with difficulty staying asleep or extreme restlessness
- Fever and sweating without other signs of illness
- Diarrhea or other digestive issues
- Stuffy nose and rapid breathing
- Seizures in severe cases
When a pregnant person uses opioids—whether prescription painkillers, heroin, or medications like methadone or buprenorphine—those substances pass through the placenta to the developing baby. The infant’s body becomes dependent on the drug. After birth, when the drug supply suddenly stops, the baby experiences withdrawal.
This condition is called Neonatal Abstinence Syndrome (NAS) or, when specifically caused by opioids, Neonatal Opioid Withdrawal Syndrome (NOWS). Between 2000 and 2012, the number of babies born with NAS increased five-fold, affecting an estimated 21,732 infants. The opioid crisis hasn’t just affected adults—it’s deeply impacting our most vulnerable population. In Florida and across Miami, healthcare providers see these tiny patients struggling through withdrawal in neonatal intensive care units. The good news? Modern treatment approaches are making a real difference, and families affected by this crisis can find compassionate, evidence-based care right here in our community.
Similar topics to infant opiate withdrawal symptoms:
- coping with opiate withdrawal
- easing withdrawal symptoms from opiates
- how long does withdrawal symptoms last from opiates
Recognizing Infant Opiate Withdrawal Symptoms and Diagnosis
When we talk about infant opiate withdrawal symptoms, we’re primarily referring to the physical and neurological signs a newborn exhibits after being exposed to opioids in the womb. Their tiny bodies, accustomed to the presence of these substances, suddenly react when the supply is cut off after birth. This is why understanding the various ways these symptoms manifest is crucial for early diagnosis and intervention. The central nervous system, which has become dependent on the opioid, becomes overstimulated, leading to a range of distressing symptoms. The baby is essentially going through a detoxification process at the most vulnerable stage of life.
The symptoms of NAS/NOWS are diverse, affecting multiple bodily systems. These can range from central nervous system excitability to significant gastrointestinal distress. It’s a challenging time for these newborns, and their cries often reflect their discomfort and confusion. The severity and type of symptoms can depend on several factors, including the specific substance used, the dosage, how long the mother used it, and the baby’s own metabolism.
Common Infant Opiate Withdrawal Symptoms
The signs of infant opiate withdrawal symptoms can appear within hours or days after birth, sometimes even weeks later, depending on the type of substance the mother used and its half-life. They can persist for days, weeks, or even months, requiring careful monitoring and management.
Here’s a detailed list of key symptoms to watch for in infants experiencing withdrawal:
-
Central Nervous System (CNS) Excitability:
- High-pitched crying: Often described as inconsolable or excessive, this is one of the most common and distressing symptoms. The cry is often shrill and continuous.
- Irritability: The baby is easily startled, restless, and difficult to soothe. They may seem constantly uncomfortable.
- Tremors or body shakes: These can be mild jitters or more pronounced shaking of the limbs, even when the baby is not cold or upset.
- Increased muscle tone (hypertonia): The baby may appear stiff or tense, with tight fists and an arched back.
- Overactive reflexes: An exaggerated startle (Moro) reflex is common, where the baby reacts strongly to sudden noises or movements.
- Seizures: In severe cases, seizures can occur, which is a serious complication requiring immediate medical intervention.
- Sleep problems: Difficulty falling or staying asleep, or very short, fragmented sleep cycles.
- Yawning and sneezing: Frequent and sometimes forceful yawning, sneezing, and hiccuping are common signs of an overstimulated nervous system.
-
Gastrointestinal (GI) Issues:
- Poor feeding: Difficulty latching, poor sucking, refusing to eat, or not consuming enough milk. This can lead to dehydration and poor weight gain.
- Vomiting: Frequent or projectile vomiting after feeds.
- Diarrhea: Loose, watery stools, often leading to severe diaper rash and dehydration.
- Difficulty gaining weight: Due to feeding problems and an increased metabolic rate from the stress of withdrawal.
-
Autonomic Nervous System (ANS) Dysfunction:
- Sweating: Often profuse, even in a cool environment.
- Fever: A low-grade fever without any other signs of infection.
- Rapid breathing (tachypnea): The baby breathes faster than normal, which can be a sign of distress.
- Stuffy nose and nasal flaring: May lead to breathing difficulties and problems with feeding.
- Skin mottling: Blotchy or discolored skin patches, indicating poor circulation.
You can learn more about general opiate withdrawal symptoms and how they manifest in adults by visiting our page on Opiate Withdrawal Symptoms.
How Doctors Diagnose Infant Opiate Withdrawal Symptoms
Diagnosing NAS/NOWS is a multi-faceted process that involves careful observation, detailed history taking, and sometimes laboratory tests. The goal is to accurately identify the condition and tailor a treatment plan that offers the best outcome for the newborn. A collaborative approach involving neonatologists, nurses, and social workers is crucial.
-
Maternal Substance Use History: This is perhaps the most crucial piece of information. Healthcare providers will ask the birthing parent about any substance use during pregnancy, including prescription opioids, illicit drugs, and even certain antidepressants or benzodiazepines. Honesty is paramount here, as this information directly guides the care team in anticipating and managing potential withdrawal. We understand this can be a difficult conversation, but it’s essential for your baby’s health. It is a conversation held with compassion and without judgment, focused solely on the well-being of the infant.
-
Physical Examination and Observation: After birth, medical staff closely monitor the newborn for any signs of withdrawal. They observe the baby’s behavior, feeding patterns, sleep, and physical responses. This observation period can last for several days, as some symptoms may not appear immediately, depending on the substance and the timing of the last dose before delivery.
-
NAS Scoring Systems: To objectively assess the severity of infant opiate withdrawal symptoms, doctors use standardized scoring systems. The traditional method has been the Finnegan Neonatal Abstinence Scoring System (FNASS). This system assigns points to various symptoms based on their intensity and frequency. A higher score indicates more severe withdrawal, guiding decisions on treatment, including medication. However, newer approaches, like the “Eat, Sleep, Console” method, are gaining traction for their focus on functional symptoms and promoting mother-infant bonding.
-
Drug Testing: To confirm exposure and identify the specific substances, various tests may be performed on the newborn:
- Urine tests: These can detect drugs in the baby’s system from recent exposure (within a few days).
- Meconium testing: Meconium, the baby’s first stool, can provide a longer history of drug exposure, reflecting use over the previous several months of pregnancy.
- Umbilical cord tissue testing: This method can also provide a history of drug exposure throughout the pregnancy and is often easier to collect than meconium.
Toxicology screens alone don’t dictate a diagnosis of NAS, nor does a negative screen rule it out, as results can sometimes be delayed or have false negatives. The clinical presentation of the baby is always the most important factor. Therefore, a comprehensive approach combining observation, scoring, and history is used to make an accurate diagnosis.
Modern Treatment for Neonatal Abstinence Syndrome
Once infant opiate withdrawal symptoms are identified, the focus shifts to providing comprehensive and compassionate care. The primary goal is to manage the baby’s withdrawal symptoms, ensure they are comfortable, and support their ability to eat, sleep, and grow. Modern treatment for NAS has evolved significantly, moving towards approaches that prioritize non-pharmacologic interventions and emphasize the crucial role of the mother-infant bond. These strategies aim to minimize the need for medication, shorten hospital stays, and reduce overall healthcare costs.
In Florida, including right here in Miami, many hospitals and neonatal units now follow updated, evidence-based guidelines for NAS/NOWS. Families admitted to local facilities often work closely with neonatologists, nurses, and social workers, while outpatient follow-up is coordinated with pediatricians and community resources. For parents who are receiving care at Summer House Detox Center, our team can collaborate with obstetric and neonatal providers in Miami to support a smoother transition from detox to prenatal or postnatal care.
The “Eat, Sleep, Console” (ESC) Approach
The “Eat, Sleep, Console” (ESC) approach represents a paradigm shift in how we manage infants with NAS/NOWS. This evidence-based model focuses on the baby’s ability to perform three key functions:
- Eat: Can the baby feed effectively and take adequate nutrition? This includes assessing their ability to latch, suck, and swallow without excessive fussiness or vomiting.
- Sleep: Can the baby sleep for at least one hour undisturbed? This indicates that their central nervous system is not overly agitated.
- Console: Can the baby be consoled within 10 minutes by a caregiver? This is a critical measure of their comfort and ability to self-regulate with support.
If a baby can do these things, even with some withdrawal symptoms, the emphasis remains on non-pharmacologic care. This approach has shown remarkable results. Clinical trials, like the Advancing Clinical Trials in Neonatal Opioid Withdrawal (ACT NOW) Eat, Sleep, Console (ESC) Clinical Trial, found that newborns cared for with ESC were medically ready for discharge 6.7 days earlier than those treated without ESC. Furthermore, only 19.5% of ESC-treated infants required opioids versus 52% of infants who did not receive ESC. This means less medication, shorter hospital stays, and more time for families to be together at home.
The ESC approach champions a family-centered care model. It promotes:
- Low-stimulation environment: Keeping the baby’s surroundings quiet, dim, and calm. This reduces sensory overload, which can exacerbate withdrawal symptoms.
- Maternal involvement: Encouraging continuous presence, skin-to-skin contact (kangaroo care), and breastfeeding (when appropriate and safe). The mother’s presence is a powerful, natural soother for the infant.
- Swaddling and gentle rocking: These are simple but highly effective comfort measures that mimic the womb environment and help soothe the baby’s overactive nervous system.
Many Florida hospitals, including those serving Miami-Dade and Broward counties, are transitioning from traditional treatment models to ESC-based protocols. Families can ask their delivering hospital whether ESC is used and how parents are involved in day-to-day care.
This is a significant difference from traditional methods, which often relied heavily on the Finnegan scoring system to determine medication needs, sometimes leading to unnecessary pharmacotherapy and longer separations between mother and child.
Traditional Care vs. Eat, Sleep, Console (ESC)
Below is a comparison of how traditional Finnegan-based care differs from the ESC approach that is increasingly used in Florida and across the United States:
| Feature | Traditional Care (Finnegan Scoring) | Eat, Sleep, Console (ESC) |
|---|---|---|
| Primary Focus | Uses the Finnegan Neonatal Abstinence Scoring System to assign a numerical score based on dozens of withdrawal signs. Medication decisions are often tied to reaching certain score thresholds. | Focuses on the baby’s functional ability to eat, sleep, and be consoled, rather than on a long symptom checklist. Treatment decisions are guided by whether the baby can meet these three goals. |
| Environment | Care frequently occurs in a Neonatal Intensive Care Unit (NICU). These units can be bright and noisy, which may overstimulate infants with NAS. Babies are sometimes separated from their parents for extended periods. | Prioritizes keeping the mother and baby together in a quiet, low-light, low-stimulation room when medically safe. Care is usually provided in the mother-baby unit or a similar setting rather than an open NICU. |
| Medication Use | Higher likelihood of pharmacologic treatment (such as morphine or methadone) because escalating Finnegan scores often trigger medication starts or dose increases. | Emphasizes non-pharmacologic comfort measures first. Medication is used only when the baby cannot eat, sleep, or be consoled despite optimal supportive care, which reduces overall opioid exposure. |
| Family Involvement | Parents may have limited contact with the infant, especially if NICU visitation is restricted or if hospital routines keep babies in central nurseries. This can increase parental stress and feelings of helplessness. | Actively involves the mother and family as primary caregivers at the bedside. Parents are encouraged and coached to use holding, skin-to-skin contact, and responsive soothing, which supports bonding and reduces guilt and stigma. |
| Hospital Stay | Hospital stays are often longer because medication is started earlier and tapered slowly based on symptom scores. Infants may require prolonged monitoring in higher-acuity units. | Hospital stays are typically shorter on average, as many infants avoid medication altogether. Earlier discharge is possible when babies consistently meet ESC goals with family-centered support. |
When Medication is Necessary
While the goal is to use non-pharmacological methods as much as possible, some infants experience withdrawal symptoms so severe that they interfere with their ability to eat, sleep, and thrive. In these cases, medication is a necessary and compassionate intervention. The primary aim is not to sedate the baby, but to manage the most distressing symptoms, such as seizures, severe irritability, and feeding difficulties, allowing the infant to rest and grow.
Commonly used medications include:
- Morphine: A short-acting opioid that is often the first-line treatment. It helps control withdrawal symptoms and can be gradually tapered as the baby stabilizes.
- Methadone: A longer-acting opioid that may be used for more severe or prolonged withdrawal, especially if the mother was on a high dose of opioids or methadone herself.
- Buprenorphine: Another long-acting opioid that is gaining popularity as a first-line treatment. Some studies suggest it may lead to shorter treatment durations and hospital stays compared to morphine.
The choice of medication depends on the specific substance the baby was exposed to, the severity of their symptoms, and the hospital’s protocol. The dose is carefully calculated based on the baby’s weight and adjusted according to their response, using scoring systems to monitor their progress. The weaning process is slow and methodical, gradually reducing the dosage over days or weeks to prevent a resurgence of withdrawal symptoms. This careful medical management is crucial for the baby’s safety and well-being.
For families in Miami and throughout Florida, coordination between maternity providers, pediatricians, and addiction treatment programs can make a major difference. When a pregnant person with opioid use disorder receives stable treatment and support before delivery, babies are more likely to have milder symptoms that can be managed with approaches like ESC. If you or a loved one is pregnant or planning a pregnancy and struggling with opioids, seeking help early through a trusted detox program can be an important step in protecting both parent and baby. To learn more about the medications that may be used in adult detox and long-term recovery, you can read about medication-assisted treatment.
