Understanding the Connection Between Opiate Withdrawal and Depression
Opiate withdrawal and depression are deeply connected, creating a challenging cycle that affects millions of Americans. When someone stops using opiates, their brain chemistry becomes severely disrupted, leading to both physical symptoms and serious mental health challenges.
Key Facts About Opiate Withdrawal and Depression:
- Physical symptoms include muscle aches, nausea, sweating, and insomnia
- Depression symptoms include persistent sadness, hopelessness, and loss of interest in activities
- Brain chemistry changes cause dopamine and serotonin imbalances during withdrawal
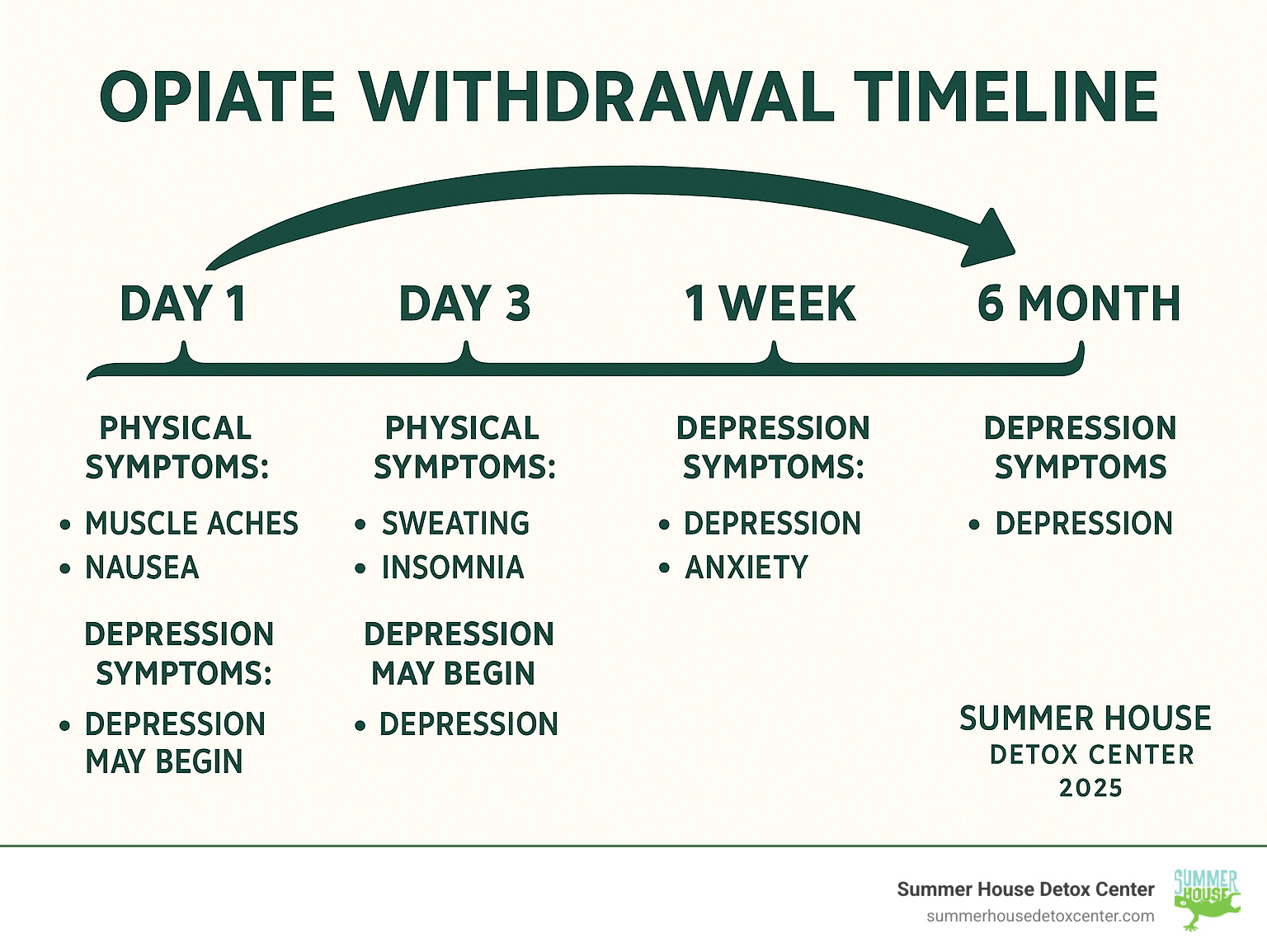
- Timeline varies but depression can last weeks or months after physical symptoms end
- Professional help is crucial for safely managing both conditions together
In Florida, the opioid crisis has hit particularly hard. From Miami’s urban communities to rural areas across the state, families are struggling with addiction and its aftermath. The good news? Recovery is possible with the right support and medical care.
When opiates flood your brain, they hijack your natural reward system. Your brain stops making its own “feel good” chemicals and relies on the drugs instead. When you stop using, your brain needs time to heal and rebalance itself. This is why many people experience severe depression during withdrawal – it’s not a sign of weakness, it’s a normal part of how addiction affects the brain.
The physical symptoms like sweating and muscle aches usually fade within days or weeks. But depression and other mental health symptoms can persist much longer. This is called Post-Acute Withdrawal Syndrome (PAWS), and it’s one of the main reasons why professional treatment is so important.
Glossary for opiate withdrawal and depression:
- opiate withdrawal symptoms
- easing withdrawal symptoms from opiates
- does suboxone help with opiate withdrawal symptoms
The Physical Onslaught: Common Opiate Withdrawal Symptoms
When you stop using opiates, your body struggles to rebalance itself. The physical symptoms of opiate withdrawal and depression hit hard because your nervous system has become dependent on these drugs to function.
While often used interchangeably, opiates (like heroin and morphine) come from the opium poppy, while opioids (like fentanyl and oxycodone) are synthetic. Your body reacts similarly to both during withdrawal. Here in Miami, we see people struggling with all types of these substances, and the withdrawal process follows a similar pattern as the brain readjusts.
The timeline and intensity depend on factors like the type of drug used (short-acting vs. long-acting), duration of use, and your overall health.
For more detailed information about what to expect, you can learn about what are the symptoms of opiate withdrawal and explore our comprehensive guide to opiate withdrawal symptoms.

Early Stage Symptoms (First 24 Hours)
Within 6 to 12 hours of the last dose, your body sends clear signals that something is wrong. Early symptoms often feel like a severe case of the flu.
- Agitation and anxiety: A feeling of restlessness and unease.
- Muscle aches: Deep, persistent pain.
- Flu-like symptoms: Runny nose, excessive yawning, and sweating, even in Miami’s air conditioning.
- Insomnia: Your body is exhausted, but your mind won’t let you rest. This is a common and frustrating symptom. Learn how to cope with insomnia after opiate detox.
These early symptoms are your body’s way of healing. Having medical support makes a significant difference in comfort and safety.
Peak Stage Symptoms (Days 2-4)
Days two through four are typically the most intense part of physical withdrawal as your body works to clear the drugs.
- Gastrointestinal distress: Severe abdominal cramping, diarrhea, nausea, and vomiting are common. This creates a serious risk of dehydration, especially in Florida’s heat.
- Physical signs: You may notice dilated pupils and frequent goosebumps, which is where the term “cold turkey” originates.
- Intense cravings: The most challenging symptom is often the overwhelming urge to use again. Your brain is screaming for the substance it depends on.
This peak period is why medical supervision is crucial. The combination of physical pain, dehydration risk, and powerful cravings is dangerous to face alone. At Summer House Detox Center, we help Miami residents get through this phase safely. The good news is that these intense physical symptoms do pass, allowing the healing process to begin.
The Unseen Struggle: Opiate Withdrawal and Depression
While physical symptoms are obvious, a quieter battle rages within. Opiate withdrawal and depression are deeply connected, creating an emotional darkness that can feel inescapable. If you’re going through this in Miami, know that over 40% of people with substance use disorders also face mental health challenges like depression.
Think of your brain’s natural “feel-good” chemicals, dopamine and serotonin. Opiates hijack their production. When you use, your brain stops making its own, relying on the external supply. When you quit, the pharmacy is empty. This leads to anhedonia—the inability to feel pleasure. Favorite activities, foods, and time with loved ones feel flat and meaningless.
This creates a vicious cycle: depression may lead to opiate use for self-medication, which then worsens the depression, making recovery feel impossible. Many in South Florida are breaking this cycle daily with the right support.
How Opiate Withdrawal Causes Depression
Understanding the link between opiate withdrawal and depression involves looking at the brain’s reward system. This system runs on dopamine, the neurotransmitter for pleasure and motivation. Opiates flood the brain with far more dopamine than any natural activity. In response, the brain reduces its own dopamine production and the number of receptors available (dopamine receptor downregulation).
When you stop using, you’re left in a chemical deficit. Your brain isn’t making enough dopamine, and the remaining receptors are less sensitive. Meanwhile, serotonin, which regulates mood and sleep, is also thrown out of balance.
This can lead to Post-Acute Withdrawal Syndrome (PAWS), where depression and anxiety persist for months. The brain needs time to heal, which is why comprehensive treatment is vital. We explore this in The Science Behind Detox: How the Body Heals from Substance Abuse.
Manifestations of Depression During Opiate Withdrawal
The depression during opiate withdrawal is more than just sadness. It’s an overwhelming state that can make daily life feel like walking through quicksand.
- Persistent sadness and hopelessness: A constant feeling of gloom and the belief that things will never get better.
- Irritability: A short fuse that can strain relationships when you need support most.
- Fatigue: A bone-deep exhaustion that sleep doesn’t fix.
- Loss of interest: Hobbies, work, and relationships feel pointless.
- Suicidal ideation: Thoughts of self-harm are a serious symptom of this chemical imbalance and require immediate professional help.
These complex symptoms are why authoritative sources like MedlinePlus stress that anyone in opiate withdrawal should be evaluated for depression. Treating both conditions together is key to recovery.
Why Professional Detox is Crucial for Co-Occurring Disorders
Facing both opiate withdrawal and depression alone is dangerous. These co-occurring disorders feed off each other, creating a storm that requires professional navigation. In Florida, many who attempt to detox at home relapse, often with fatal consequences due to lowered tolerance.
Dual diagnosis treatment, which addresses addiction and mental health simultaneously, is life-saving. Without professional support, the hopelessness of withdrawal depression often drives people back to using.
Medically supervised detox provides a crucial safety net. Medical staff monitor your vitals, manage complications like dehydration, and offer support when depression feels unbearable. It’s about keeping you stable while your brain heals. You wouldn’t treat a broken leg at home; the same logic applies to this complex medical condition. Our Opiate Detox Program is designed to address these interconnected challenges. Learn more about What are the risks of quitting opiates cold turkey?.

Medication-Assisted Treatment (MAT)
MAT uses FDA-approved medications to stabilize brain chemistry, allowing you to focus on healing. It’s not trading one addiction for another; it’s providing your brain with support as it recovers.
- Buprenorphine (e.g., Suboxone): Reduces cravings and withdrawal symptoms without a high. Learn Does Suboxone help with opiate withdrawal symptoms?.
- Methadone: Works similarly but requires visits to a licensed clinic, providing helpful structure.
- Naltrexone: Blocks the effects of opioids, preventing a high if relapse occurs. It can only be started after detox is complete.
- Symptom-Relief Medications: Gabapentin can calm restlessness and anxiety, while Clonidine helps with physical symptoms like sweating and muscle aches.
These medications are prescribed and monitored by professionals. See Which medications are used in opiate detox?.
The Importance of Integrated Care
Treating opiate withdrawal and depression requires an integrated approach where the entire treatment team works together.
- Individual and Group Therapy: Therapy helps you unpack the relationship between your substance use and mental health. Group sessions provide a powerful connection with peers who understand your struggle.
- Holistic Approaches: Yoga, meditation, and art therapy address your well-being by calming the mind and body, helping you process emotions in new ways.
For Florida residents, professional, compassionate care is essential. Find out Who needs opiate detox in Florida? to see if this path is right for you.
Life After Withdrawal: Managing Long-Term Mental Health
Completing detox is a monumental achievement, but it’s the beginning of the journey. While acute physical symptoms fade, psychological effects like depression can linger. This is where the real work of managing long-term mental health begins—building a new life with healthy coping strategies and a strong support system.
Long-term recovery means actively creating a lifestyle that supports sobriety and mental well-being. It’s about learning to steer life’s challenges without substances. In Miami, finding the right resources is key. You can explore Opiate Detox Centers: How to Find the Best Support for Your Needs to guide your decision.

Coping with Post-Acute Withdrawal Syndrome (PAWS) and Depression
Even after detox, your brain is still healing. Post-Acute Withdrawal Syndrome (PAWS) is a slow-motion recovery process where psychological and emotional symptoms can surface for months or even years. This is especially challenging when dealing with opiate withdrawal and depression.
PAWS symptoms often include mood swings, anxiety, persistent depression, sleep disturbances, irritability, and low energy. Cravings can also pop up unexpectedly. Understanding that PAWS is a normal part of the brain’s healing process is crucial, as its symptoms can lead to relapse if not managed.
Proven ways to manage PAWS and depression include:
- Exercise and Nutrition: Physical activity helps your brain produce its own feel-good chemicals. A healthy diet supports brain health and rebalances chemistry.
- Mindfulness and Routine: Meditation can help you stay grounded during emotional shifts. Establishing consistent routines provides stability for your healing brain.
- Cognitive Behavioral Therapy (CBT): CBT teaches you to identify and change the negative thought patterns that fuel depression and cravings, giving you practical coping tools.
Finding Support and Resources
You don’t have to face long-term recovery alone. Building a strong support system is essential.
- Peer Support Groups: Narcotics Anonymous (NA) offers fellowship with people who understand your journey. SMART Recovery uses science-based tools to help you gain independence from addiction.
- National Helplines: The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a helpline and online resources at www.samhsa.gov/find-support. For immediate crisis support, the 988 Suicide & Crisis Lifeline is available 24/7 by calling or texting 988.
- Family Therapy: Addiction affects the whole family. Therapy can help rebuild trust, improve communication, and establish healthy boundaries.
Here in Miami and across Florida, local support groups and professionals understand the unique challenges of our environment. Don’t hesitate to reach out; asking for help is a sign of strength.
Frequently Asked Questions about Opiate Withdrawal
When you’re facing opiate withdrawal and depression, it’s natural to have questions swirling through your mind. We’ve heard these concerns countless times from people just like you who are considering taking that brave first step toward recovery. Let’s address some of the most pressing questions we hear from folks here in Miami and throughout Florida.
Is opiate withdrawal deadly?
While opiate withdrawal itself is generally not directly life-threatening like alcohol withdrawal, its complications can be dangerous. Severe vomiting and diarrhea can lead to life-threatening dehydration and electrolyte imbalances.
However, the single biggest danger is the increased risk of overdose after relapse. During detox, your tolerance drops significantly. If you return to using the same amount as before, your body can’t handle it, which is often fatal. This is why medical supervision is critical. We explore this further in Is opiate withdrawal deadly?.
How long do withdrawal symptoms last?
There’s no one-size-fits-all answer, but there is a general timeline. The acute phase, with intense physical symptoms, typically lasts 1-2 weeks.
The duration is influenced by the type of opiate used, how long and how much was used, and your overall physical and mental health. Psychological symptoms, especially depression, can persist much longer through Post-Acute Withdrawal Syndrome (PAWS), which can last for months or even up to two years. This is why ongoing support is so important.
Can you use herbal remedies for opiate withdrawal?
In the face of withdrawal, “natural” remedies can sound appealing. However, the Food and Drug Administration (FDA) has not approved any herbal remedies for treating opiate withdrawal because there is no scientific evidence that they are safe or effective.
Some products, like kratom, are marketed as solutions but can cause their own addiction and withdrawal. Many herbal products are unregulated and may be contaminated. When dealing with opiate withdrawal and depression, you deserve proven, evidence-based treatments. Relying on unproven methods can be dangerous and delay real help. Learn more on our page about Herbal Remedies for Opiate Withdrawal Symptoms. Your life is too precious to gamble on unproven remedies.
Begin Your Recovery Journey in Miami
The connection between opiate withdrawal and depression creates one of the most challenging battles anyone can face. Throughout this journey, we’ve explored how your brain’s chemistry gets disrupted when opiates are removed, leading to both crushing physical symptoms and profound emotional pain. The muscle aches and nausea are tough enough, but when combined with the hopelessness and sadness that depression brings, it can feel like an impossible mountain to climb.
Here in Miami and throughout Florida, we’ve witnessed the devastating impact of the opioid crisis on our communities. But we’ve also seen something beautiful: recovery happening every single day. Real people, with real struggles just like yours, finding their way back to health and happiness.
At Summer House Detox Center, we understand that your journey through opiate withdrawal and depression isn’t just about managing symptoms – it’s about reclaiming your life. Our team knows that healing happens best when you’re treated with dignity, compassion, and genuine care. Many of our staff members have walked similar paths themselves, which means they truly understand what you’re going through.
The first step is often the hardest, but you don’t have to take it alone. Our personalized approach means we create a treatment plan specifically for you – considering your unique situation, your health history, and your goals for recovery. We believe in medically supervised detox because we know it’s not just safer, it’s more effective for long-term success.
Taking that first step toward healing requires incredible courage, and we honor that bravery. You’ve already shown tremendous strength by learning about the connection between withdrawal and depression. Now let us help you turn that knowledge into action.
Recovery is possible. Hope is real. And professional help makes all the difference.
If you’re ready to break free from the cycle of addiction and find relief from depression, we’re here to support you every step of the way. Your journey to healing can begin today.
Find compassionate, medically-supervised opiate detox services today
