Understanding Your Options for Opiate Withdrawal Treatment
Medicine for opiate withdrawal symptoms includes several FDA-approved options that help manage the physical and psychological discomfort of stopping opioid use. If you’re searching for immediate answers, here’s what you need to know:
Main Medication Categories:
- Opioid Agonists (Methadone, Buprenorphine) – Reduce cravings and ease withdrawal symptoms by activating the same brain receptors as opioids, but in a controlled way
- Alpha-2 Adrenergic Agonists (Clonidine, Lofexidine) – Help manage physical symptoms like sweating, rapid heartbeat, and muscle aches
- Opioid Antagonists (Naltrexone) – Block opioid effects and prevent relapse after detox is complete
- Symptomatic Relief Medications – Treat specific symptoms like nausea, diarrhea, insomnia, and anxiety
Withdrawal from opiates is rarely life-threatening, but it’s incredibly uncomfortable and difficult to manage alone. The research is clear: detoxification on its own, without medication, significantly increases your risk of relapse, overdose, and overdose death.
This is where many people feel stuck. You want to stop using, but the fear of withdrawal keeps you trapped. Past attempts may have failed because the symptoms were too severe, or because you tried to quit “cold turkey” without proper support.
Here in Florida, and specifically at facilities like Summer House Detox Center in Miami, medically supervised detox offers a safer path. With 24/7 medical monitoring, personalized medication protocols, and compassionate care, withdrawal becomes manageable. You don’t have to suffer alone.
The truth is simple: medically supervised withdrawal is not just more comfortable—it’s more effective. Studies show that medication-assisted treatment reduces overdose risk and helps more people complete detox successfully. After withdrawal, your tolerance drops dramatically, making relapse incredibly dangerous. Professional support helps you steer this critical period safely.
This guide will walk you through every medication option available, explain how medically supervised detox works in Florida, and show you what to expect from treatment. Whether you’re considering detox for yourself or a loved one, understanding your options is the first step toward recovery.
Medicine for opiate withdrawal symptoms terms to learn:
- does gabapentin help with opiate withdrawal symptoms
- does suboxone help with opiate withdrawal symptoms
- herbal remedies for opiate withdrawal symptoms
Understanding Opiate Withdrawal Symptoms and Diagnosis
Opioid withdrawal symptoms can be incredibly challenging, both physically and psychologically. These symptoms arise because the body has become physiologically dependent on opioids. When the opioid supply is stopped or significantly reduced, the body reacts, trying to re-establish a state of balance. This biological response is why managing withdrawal symptoms can be so difficult without professional help.

What are opioid withdrawal symptoms and why are they difficult to manage?
The symptoms of opioid withdrawal can feel like an intense, prolonged flu combined with severe emotional distress. They include a range of physical and psychological manifestations:
- Physical symptoms often include muscle aches, bone pain, runny nose, watery eyes, sweating, chills, goosebumps (piloerection), yawning, nausea, vomiting, diarrhea, abdominal cramps, and dilated pupils. In severe cases, high blood pressure and rapid heart rate (tachycardia) can occur.
- Psychological symptoms can involve intense drug craving, anxiety, restlessness, irritability, insomnia, and dysphoric mood.
These symptoms are difficult to manage because they are not just uncomfortable; they are driven by significant changes in brain chemistry. The locus coeruleus, a region in the brain, plays a principal role in triggering many of these symptoms. Chronic opioid use alters the balance of neurotransmitters, and when opioids are removed, this balance is thrown into disarray, leading to the intense and widespread physical and emotional distress. The sheer intensity and persistence of these symptoms make it incredibly hard for individuals to endure withdrawal without support, often leading to relapse to alleviate the suffering.
At Summer House Detox Center, we understand that accurately assessing these symptoms is crucial for effective treatment. We use validated withdrawal scales, such as the Clinical Opiate Withdrawal Scale (COWS), to objectively measure the severity of withdrawal. This assessment helps our medical team tailor the perfect medicine for opiate withdrawal symptoms to your specific needs. The COWS scale, which evaluates 11 signs and symptoms, provides a score that guides our treatment decisions, ensuring you receive appropriate care.
For a more detailed understanding of what to expect, you can read our guide on What Are the Symptoms of Opiate Withdrawal?.
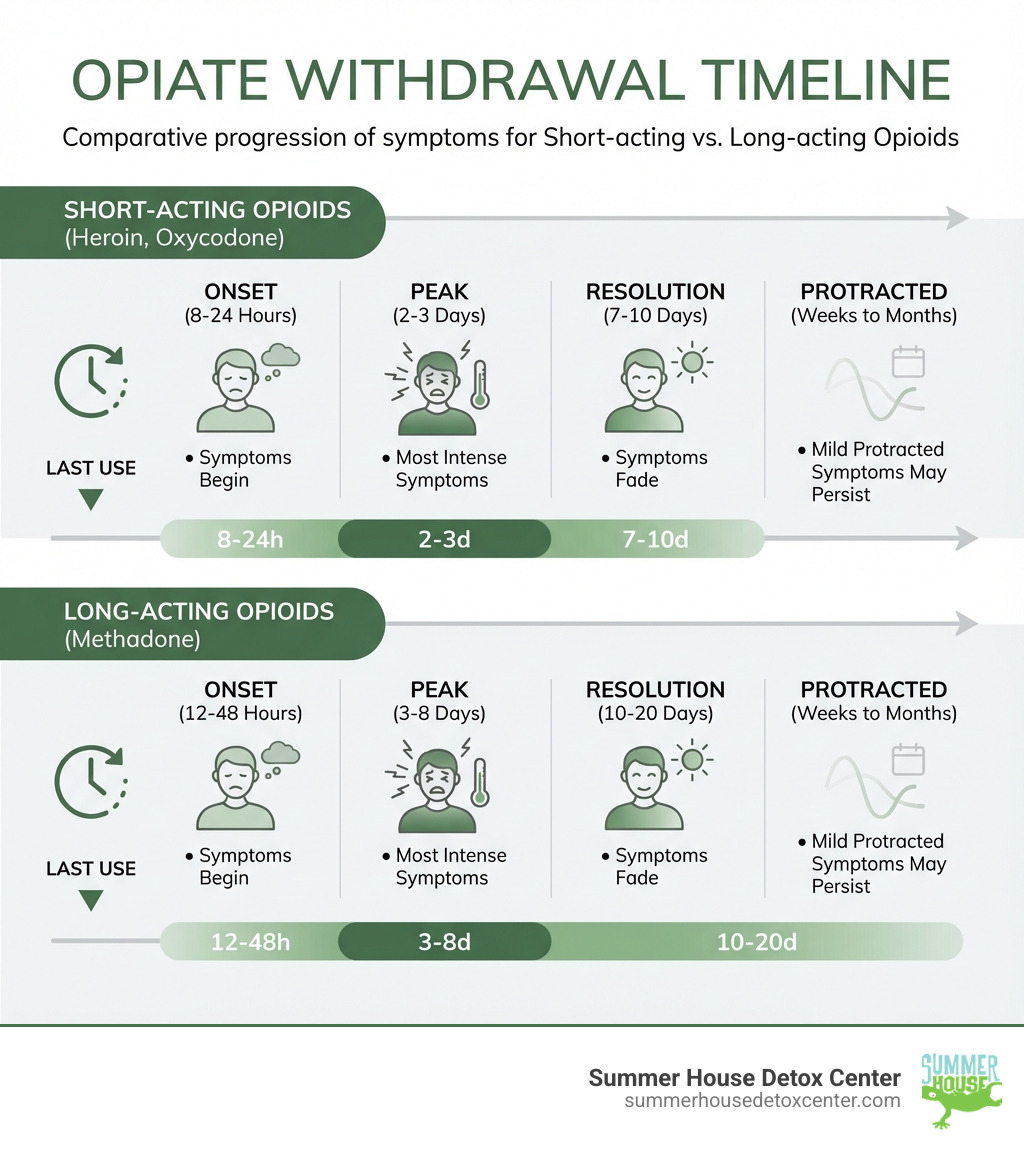
The duration of withdrawal symptoms varies significantly depending on the type of opioid used, the dose, and the duration of use. For short-acting opioids like heroin or oxycodone, symptoms can start within 8-24 hours after the last dose, peak around 2-3 days, and generally resolve within 7-10 days. For longer-acting opioids like methadone, symptoms might not appear until 12-48 hours after the last dose, peak later (3-8 days), and can last for 10-20 days. Even after the acute phase, some less severe symptoms, known as protracted withdrawal, can linger for weeks to months. Our article How Long Does It Take to Withdraw From Opiates? provides more insights into this timeline.
FDA-Approved Medicine for Opiate Withdrawal Symptoms
Medication-assisted treatment (MAT) is a cornerstone of modern opioid withdrawal management. It’s not about replacing one addiction with another; it’s about using FDA-approved medicine for opiate withdrawal symptoms to safely and comfortably manage the detox process. This approach has been shown to reduce the risk of overdose and overall mortality, making it the recommended standard of care.
At Summer House Detox Center, our professional Opiate Detox Center in Miami, FL, uses these medications as part of a comprehensive, medically supervised detox program. We understand that each individual’s needs are unique, and our experienced medical team crafts personalized treatment plans.
Here are the main categories of medications we use, along with common symptomatic relief medications:
- Opioid Agonists: Methadone, Buprenorphine
- Alpha-2 Adrenergic Agonists: Clonidine, Lofexidine (LUCEMYRA)
- Opioid Antagonists: Naltrexone (used post-detox)
Symptomatic Relief Medications for specific withdrawal symptoms include:
- Anti-nausea medications (e.g., promethazine, metoclopramide) for gastrointestinal distress.
- Anti-diarrheal medications (e.g., loperamide) for severe diarrhea.
- Non-steroidal anti-inflammatory drugs (NSAIDs) or acetaminophen for muscle aches and pain.
- Sleep aids (non-addictive options) for insomnia.
- Anti-anxiety medications (e.g., diazepam, though used cautiously and typically short-term in a supervised setting) for severe anxiety and agitation.
Opioid Agonists: Methadone and Buprenorphine
Opioid agonists are medications that bind to the same opioid receptors in the brain as illicit opioids, but they do so in a controlled way to prevent withdrawal symptoms and reduce cravings without producing the same euphoric high. This helps stabilize the individual during detox.
- Methadone: As a full opioid agonist, methadone activates opioid receptors completely. It’s a long-acting synthetic opioid that can significantly reduce withdrawal symptoms and cravings. Methadone is typically administered through SAMHSA-certified opioid treatment programs, ensuring careful monitoring and dosage adjustments. It’s effective for both short-term withdrawal management and long-term maintenance treatment.
- Buprenorphine: This is a partial opioid agonist, meaning it activates opioid receptors less completely than full agonists. Buprenorphine effectively reduces cravings and withdrawal symptoms with a lower risk of euphoria, sedation, and overdose compared to full agonists. It’s often combined with naloxone (e.g., in Suboxone) to deter misuse; if injected, the naloxone component can precipitate withdrawal, making it less appealing for illicit use. Buprenorphine can be prescribed in various clinical settings by qualified clinicians, including here in Florida, after the Mainstreaming Addiction Treatment (MAT) Act eliminated the DATA-Waiver (X-Waiver) program, making it more accessible.
One critical aspect of buprenorphine use is the timing of its induction. To avoid “precipitated withdrawal” (a sudden and severe onset of withdrawal symptoms), buprenorphine should only be started when clear signs of objective withdrawal are present, typically after a COWS score of 6 or more. For short-acting opioids, this usually means waiting 12-18 hours after the last dose, and for long-acting opioids, 24-48 hours. Our detox protocols at Summer House Detox Center in Miami, FL, are designed to ensure safe and effective buprenorphine induction.
Alpha-2 Adrenergic Agonists: Clonidine
Alpha-2 adrenergic agonists are non-opioid medications that play a vital role in managing the autonomic nervous system symptoms of opioid withdrawal. These are the “fight or flight” responses that manifest as many of the uncomfortable physical symptoms.
- Clonidine: This medication helps to reduce symptoms like anxiety, agitation, muscle aches, sweating, runny nose, and cramping by calming the overactive nervous system. While highly effective for these physical symptoms, clonidine does not directly address opioid cravings. A key consideration when using clonidine is its effect on blood pressure; it can cause hypotension (low blood pressure). Our medical team carefully monitors blood pressure, and doses may be adjusted or withheld if blood pressure drops too low.
- Lofexidine (LUCEMYRA): This is the only FDA-approved, non-opioid medicine specifically for opioid withdrawal symptoms. Like clonidine, lofexidine is an alpha-2 adrenergic agonist that helps alleviate many of the same physical withdrawal symptoms. Research shows that lofexidine has less effect on blood pressure than clonidine, making it a preferred choice for outpatient opioid withdrawal management where blood pressure monitoring might be less intensive. LUCEMYRA is highlighted as providing the biggest improvement in symptom relief when symptoms are most severe, offering a significant advantage in patient comfort.
Both clonidine and lofexidine are essential components of a comprehensive medicine for opiate withdrawal symptoms regimen, providing much-needed relief from the distressing physical effects of withdrawal.
Opioid Antagonists: The Role of Naltrexone
Naltrexone is different from opioid agonists and alpha-2 adrenergic agonists because it doesn’t alleviate withdrawal symptoms. Instead, it serves a crucial role after detoxification is complete, primarily for relapse prevention and long-term abstinence.
- How it works: Naltrexone is an opioid antagonist, meaning it binds to opioid receptors but does not activate them. Instead, it blocks them, preventing any opioids from producing their euphoric and sedative effects. This effectively removes the “reward” associated with opioid use, helping to reduce cravings and prevent relapse.
- Timing is key: The importance of timing with naltrexone cannot be overstated. It must only be administered after an individual has completely detoxified from opioids. If naltrexone is taken while opioids are still in the system, it can trigger sudden and severe “precipitated withdrawal.” For this reason, individuals typically need to be opioid-free for 7-10 days (for short-acting opioids) or 10-14 days (for long-acting opioids) before starting naltrexone.
- Forms: Naltrexone is available in oral form and as an extended-release injectable (Vivitrol), which can be administered monthly, potentially increasing treatment retention.
- Long-term support: While naltrexone is not a medicine for opiate withdrawal symptoms in the acute sense, it is an invaluable tool for maintaining recovery. It helps individuals maintain abstinence by blocking the effects of opioids, allowing them to focus on psychosocial interventions and build a new, sober life. At Summer House Detox Center, after successful completion of detox, we incorporate naltrexone into our aftercare planning, if appropriate, to support long-term abstinence. You can learn more about its role in treatment in our guide on Which Medications Are Used in Opiate Detox?.
The Medically Supervised Detox Process in Florida
Medically supervised opioid withdrawal, often called detoxification, is the process of safely and comfortably managing the physical symptoms of opioid dependence when someone stops using opioids. It’s the essential first step in a longer journey of recovery, and it’s best done in a specialized facility like Summer House Detox Center in Miami, FL.
What is medically supervised opioid withdrawal and what is its primary purpose?
Its primary purpose is to safely and successfully transition the patient to long-term treatment for opioid use disorder (OUD). Medically supervised detox involves 24/7 medical monitoring, personalized medication protocols, and a supportive environment to ensure your safety and comfort. This contrasts sharply with attempting to withdraw at home or “cold turkey,” which can be dangerous and often unsuccessful.
Choosing Florida for opiate detox offers several advantages, including access to high-quality facilities like ours, beautiful and serene environments conducive to healing, and a strong network of recovery support services. For more information, explore Why Choose Florida for Opiate Detox. Our Opiate Detox Program is designed to provide comprehensive care from admission through aftercare planning.
Indications and Considerations for Medically Supervised Withdrawal
When is medically supervised opioid withdrawal indicated?
Medically supervised withdrawal is indicated for anyone who is physiologically dependent on opioids and wishes to stop using them. This includes individuals who have been using prescription opioids, illicit opioids, or even those on long-term opioid pain medication who wish to taper off. The severity of dependence, duration of use, and overall health status all play a role in determining the need for supervised detox. Our team assesses Who Needs Opiate Detox in Florida? with a thorough evaluation upon admission.
Are there specific considerations for vulnerable populations, such as pregnant women, during opioid withdrawal?
Yes, absolutely. Special populations require custom approaches. For pregnant women dependent on opioids, for instance, rapid withdrawal is generally not recommended due to potential risks to both the mother and the fetus. Instead, methadone maintenance treatment is often the recommended approach, as it stabilizes the mother and supports a healthier pregnancy outcome.
What are the indications and contraindications for medically supervised opioid withdrawal?
- Indications: Opioid dependence, desire to discontinue opioid use, risk of severe withdrawal symptoms, co-occurring medical or mental health conditions that complicate withdrawal, and a need to transition to long-term OUD treatment.
- Contraindications: While rare, certain severe medical conditions might require stabilization before detox, or specific circumstances might make a particular medication regimen unsuitable. These are always assessed by our medical professionals.
- Co-occurring disorders: Individuals with co-occurring mental health disorders (e.g., depression, anxiety) or other substance use disorders (e.g., alcohol, benzodiazepines) require integrated care. Managing these conditions during detox is crucial, as they can complicate the withdrawal process and increase the risk of relapse.
A Typical Regimen: What to expect from a medicine for opiate withdrawal symptoms
When you come to Summer House Detox Center, our medical team will conduct a thorough assessment to create a personalized treatment plan. This plan will typically involve a combination of medicine for opiate withdrawal symptoms and supportive care.
- Buprenorphine induction protocol: If buprenorphine is chosen, our team will carefully time its administration. We wait until objective signs of withdrawal are clearly present (guided by the COWS score) to avoid precipitated withdrawal. The initial dose will be carefully monitored, and subsequent doses adjusted as needed to manage symptoms effectively.
- Tapering schedules: For medications like buprenorphine or methadone, a gradual tapering schedule is often implemented. This means the dosage is slowly reduced over several days, allowing your body to adjust more gently and minimizing discomfort.
- Symptomatic medications: Throughout the detox process, we provide medications to alleviate specific, uncomfortable symptoms. This might include anti-nausea drugs for stomach upset, anti-diarrheals, non-opioid pain relievers for muscle aches, and non-addictive sleep aids to help with insomnia. If you’re wondering Does Gabapentin Help With Opiate Withdrawal Symptoms?, our medical staff can discuss its potential role in your personalized plan. We also have resources on How Can I Cope With Insomnia After Opiate Detox? to support your comfort.
- Ensuring patient comfort: Our focus is on making the detox process as comfortable and dignified as possible. This includes a serene environment, 24/7 medical supervision, and compassionate support from our staff, some of whom have personal recovery experience. We prioritize hydration and nutrition to support your body through the process.
Beyond Medication: The Importance of Psychosocial Support
While medicine for opiate withdrawal symptoms is vital for managing the acute physical discomfort, it’s crucial to understand that detox is just the initial step. Medically supervised withdrawal alone does not generally result in sustained abstinence from opioids. Its primary purpose is to prepare you for the next phase of recovery.
- Detox as the first step: Once physical withdrawal symptoms are managed, the real work of recovery begins. This involves addressing the underlying psychological and behavioral factors that contributed to opioid use disorder.
- Individual therapy: Our program emphasizes individual counseling, where you’ll work one-on-one with a therapist to explore triggers, develop coping mechanisms, and address any co-occurring mental health issues.
- Group counseling: Participating in group therapy provides a supportive community where you can share experiences, learn from others, and build a sense of connection.
- Aftercare planning: Before you leave our facility, we work with you to develop a comprehensive aftercare plan. This plan is custom to your needs and may include recommendations for continued therapy, support groups (like Narcotics Anonymous or SMART Recovery), sober living arrangements, and ongoing medication management (e.g., naltrexone).
- Transition to long-term recovery: Our goal is to help you successfully transition from detox to long-term recovery. This holistic approach, combining medical care with robust psychosocial support, significantly increases your chances of achieving lasting sobriety. Florida offers a wide array of recovery resources, and we help connect you with the best options. This comprehensive approach is what defines effective Opiate Detox Treatment.
Frequently Asked Questions about Opiate Withdrawal Medications
We often hear many questions from individuals and their families about the detox process and the role of medicine for opiate withdrawal symptoms. Here, we address some of the most common concerns.
Is opiate withdrawal deadly?
This is a critical question, and the answer requires nuance. Is Opiate Withdrawal Deadly? https://summerhousedetoxcenter.com/is-opiate-withdrawal-deadly/ While opioid withdrawal syndrome is typically not directly life-threatening, it is a serious condition that can lead to dangerous complications. The intense discomfort and physical symptoms can pose significant risks if not medically managed.
- Complications vs. direct fatality: Direct fatality from opioid withdrawal itself is rare. However, severe vomiting and diarrhea can lead to extreme dehydration and electrolyte imbalances, which can be life-threatening. Aspiration pneumonia (inhaling vomit into the lungs) is another potential serious complication.
- Increased overdose risk post-detox: Perhaps the most significant danger associated with unmanaged withdrawal is the dramatically increased risk of overdose after detox. Once you’ve gone through withdrawal, your body’s tolerance to opioids significantly decreases. If you relapse and use the same amount of opioids you used before detox, the risk of fatal overdose is extremely high.
- Why medical supervision is critical: Medically supervised detox, like that offered at Summer House Detox Center, mitigates these risks. Our 24/7 medical monitoring ensures that any complications are immediately addressed, and the use of medicine for opiate withdrawal symptoms makes the process safer and more tolerable, reducing the likelihood of severe dehydration or other dangerous outcomes. This also sets the stage for continued treatment, which is essential for preventing relapse and subsequent overdose.
How does medically supervised withdrawal compare to quitting ‘cold turkey’?
The difference between medically supervised withdrawal and attempting to quit “cold turkey” is stark and can mean the difference between success and dangerous failure.
- Safety: Medically supervised detox prioritizes your safety. Our medical team monitors your vital signs, manages complications, and administers medicine for opiate withdrawal symptoms to prevent severe distress. Quitting cold turkey, especially from significant opioid dependence, carries high risks of severe dehydration, aspiration, and other medical emergencies without any professional oversight.
- Comfort: The primary goal of medical detox is to make withdrawal as comfortable as possible. Medications significantly reduce the severity of physical and psychological symptoms. Cold turkey withdrawal is notoriously agonizing, often described as the worst flu imaginable, multiplied by ten, leading to immense suffering.
- Symptom management: In a supervised setting, every symptom, from nausea to anxiety, can be addressed with appropriate medication and care. Cold turkey offers no such relief, leaving individuals to endure the full brunt of withdrawal symptoms alone.
- Relapse rates: The intense discomfort of cold turkey withdrawal often leads to very high relapse rates. People simply cannot tolerate the pain and return to opioid use for relief. Medically assisted detox makes completing withdrawal significantly more likely.
- Overdose risk: As mentioned, post-detox, tolerance is greatly reduced. Relapse after cold turkey withdrawal is incredibly dangerous due to the heightened risk of overdose. Medical detox transitions you to a safer state and prepares you for long-term treatment, which helps prevent relapse.
- Success in completing detox: Studies show that completion of treatment is significantly more likely with alpha-2 adrenergic agonists (like clonidine or lofexidine) compared with placebo. This highlights the effectiveness of medication in helping individuals get through the withdrawal phase.
- Professional support vs. isolation: At Summer House Detox Center, you are never alone. You have the support of experienced medical professionals and compassionate staff. Quitting cold turkey often means facing the most challenging experience of your life in isolation, which can be psychologically devastating. Our article What Are the Risks of Quitting Opiates Cold Turkey? digs deeper into these dangers.
Can I detox from opiates at home?
The idea of detoxing from opiates in the comfort of your own home might seem appealing, but the reality is that it carries significant risks and a low success rate.
- Risks of at-home detox: Without medical supervision, you are vulnerable to severe dehydration, electrolyte imbalances, and other medical complications. The intense physical and psychological symptoms can be overwhelming and dangerous.
- Severe discomfort: Attempting to detox at home means enduring the full, unmitigated force of withdrawal symptoms. This level of discomfort is often unbearable and can lead to severe emotional distress, panic attacks, and even thoughts of self-harm.
- High failure rate: The sheer agony of unmanaged withdrawal makes it incredibly difficult to complete detox at home. Most individuals relapse simply to alleviate the excruciating symptoms, often within hours or days.
- Lack of immediate support: In a medical detox setting, help is always just a call away. If a symptom becomes severe or a complication arises, our medical team can intervene immediately. At home, you lack this critical, immediate support.
- Why professional detox is the standard of care: Professional, medically supervised detox centers like Summer House Detox Center provide the safest and most effective environment for opiate withdrawal. We offer 24/7 medical monitoring, personalized medicine for opiate withdrawal symptoms, and a supportive environment designed to maximize comfort and minimize risks. Our guide Are At-Home Opiate Detox Kits Safe? further explains why professional care is paramount.
Conclusion: Your First Step Towards Recovery in Miami
Understanding the role of medicine for opiate withdrawal symptoms is your first powerful step toward healing. We’ve seen how these medications, administered under medical supervision, can transform a terrifying and dangerous process into a manageable and safe one. Detox is not just about stopping opioid use; it’s about doing so in a way that respects your body, your mind, and your future.
At Summer House Detox Center, we firmly believe that detox is the crucial beginning of a long-term recovery journey. Our personalized, medically supervised detox programs in Miami, FL, are designed with your comfort, dignity, and ultimate success in mind. Our experienced staff, some of whom are in recovery themselves, provide compassionate, round-the-clock care, ensuring that you are supported every step of the way.
If you or a loved one in Florida is ready to take the first step towards a life free from opioid dependence, we are here to help. Learn more about our comprehensive Detox Services: Opiate Detox and how we can support your journey to lasting recovery.

