When Two Substances Converge: Understanding the Detox Challenge
Does benzodiazepines detox protocol cover alcohol as well as a dedicated alcohol withdrawal protocol? The short answer is no—these two substances require different approaches, and attempting to use a single protocol for both can be dangerous.
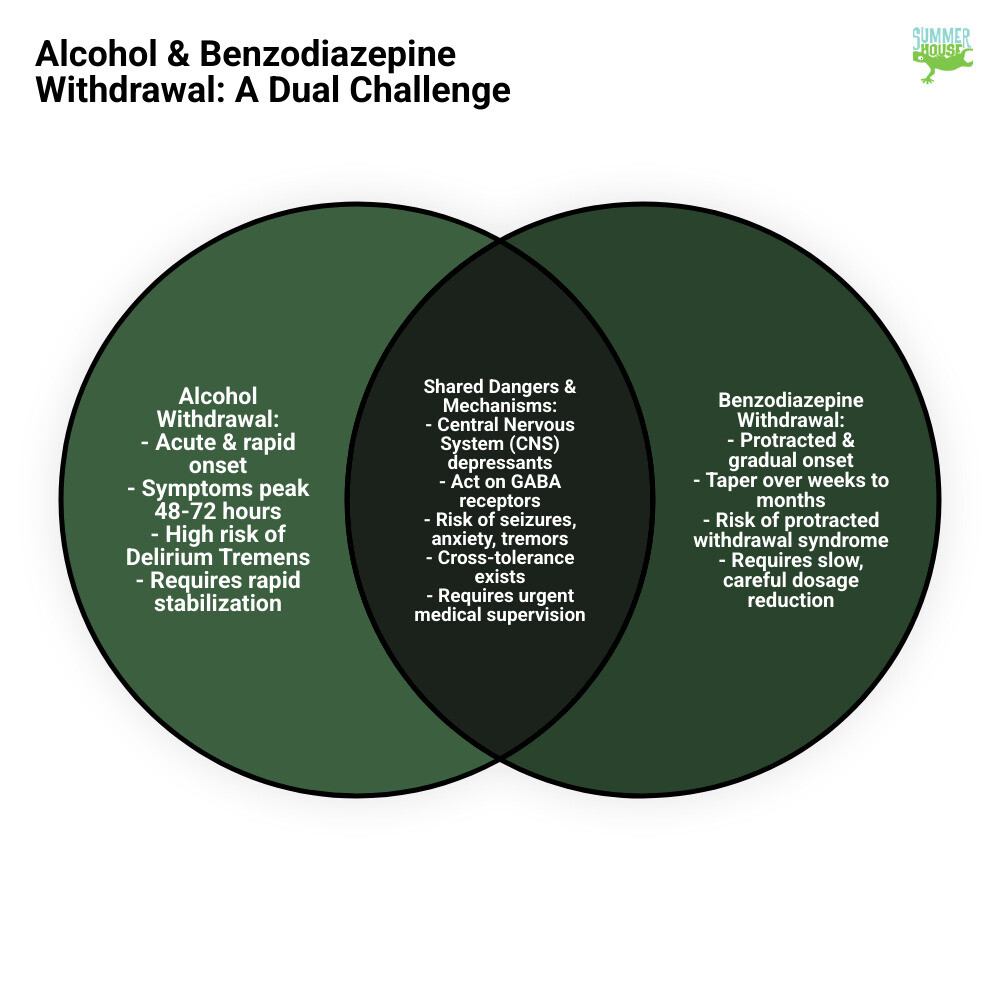
Key Differences:
- Benzodiazepine detox requires a slow, gradual taper over weeks or months to prevent severe withdrawal
- Alcohol detox addresses acute withdrawal symptoms that peak within 48-72 hours
- Combined dependence demands an integrated approach that addresses both substances sequentially, not simultaneously
- Cross-tolerance exists between benzos and alcohol, but this doesn’t mean one protocol works for both
If you’re searching for help in Miami or throughout Florida, understanding why a one-size-fits-all approach doesn’t work could save your life.
Both alcohol and benzodiazepines act on the same brain system—the GABA receptors. This shared pathway creates dangerous complications when someone is dependent on both. While traditional alcohol withdrawal protocols often use benzodiazepines as medication, this is fundamentally different from treating benzodiazepine dependence itself.
Research shows that up to 71% of people presenting for alcohol detox experience significant withdrawal symptoms, and between 5-15% will develop seizures or delirium tremens. When benzodiazepine dependence is added to the mix, the risks multiply. Yet many people assume that because these substances work similarly in the brain, one detox protocol should handle both.
The reality is more complex. Someone withdrawing from alcohol needs rapid stabilization—symptoms can become life-threatening within 48 hours. Someone withdrawing from benzodiazepines, however, needs a careful, extended taper that can take weeks or even months. Rush a benzo taper, and you risk seizures. Slow down alcohol detox, and you risk delirium tremens.
This complexity is exactly why medical supervision in a specialized facility matters so much, particularly for residents in Florida seeking safe, evidence-based care.
The Dangers of Dual Dependence: Why Alcohol and Benzos are a Risky Mix
When someone is dependent on both alcohol and benzodiazepines, stopping either one is like walking a tightrope without a safety net. Both substances slow down your brain’s activity—they’re what doctors call central nervous system depressants. Your brain adapts to their presence over time, adjusting its chemistry to compensate. When you suddenly remove them, your brain doesn’t just return to normal. It rebounds hard, going into overdrive.
This rebound effect isn’t just uncomfortable—it can be life-threatening. We’ve walked alongside countless individuals in our Miami facility through these withdrawal symptoms, and we’ve seen how frightening they can be. The shared symptoms between alcohol and benzodiazepine withdrawal read like a warning label: intense anxiety that makes you feel like you’re crawling out of your skin, tremors that make simple tasks impossible, profuse sweating, heart palpitations, and the most dangerous complications—seizures and Delirium Tremens (DTs).
Here in Florida, where the heat can make physical symptoms even more uncomfortable, the critical need for medical supervision becomes crystal clear. This isn’t something you want to face alone in your home, no matter how strong you think you are.
Alcohol vs. Benzodiazepine Withdrawal Timelines
The question does benzodiazepines detox protocol cover alcohol as well as a dedicated alcohol protocol becomes clearer when you understand how differently these substances behave during withdrawal.
Alcohol withdrawal moves fast—sometimes dangerously fast. Within 6-12 hours of your last drink, you might notice minor symptoms like restlessness, anxiety, and shaky hands. By 12-24 hours, some people start experiencing hallucinations—seeing, hearing, or feeling things that aren’t there. The risk of seizures typically peaks between 24-48 hours, though they can happen anywhere from two hours to five days after stopping. Then comes the most serious threat: Delirium Tremens, usually arriving 48-72 hours after the last drink. DTs bring severe confusion, disorientation, vivid hallucinations, and a racing heart. Without treatment, DTs can be fatal.
Benzodiazepine withdrawal follows a different rhythm entirely. While acute symptoms might begin within hours or days depending on which benzo you’ve been taking, the overall process stretches out much longer. A safe benzodiazepine taper isn’t measured in days—it’s measured in weeks, months, or sometimes even longer. Rush it, and you risk severe symptoms that can last for months, including seizures and psychological distress that can feel unbearable.
This is exactly why Florida-based detox specialists need to assess each person individually. The timelines don’t line up, the pacing is completely different, and trying to force them into a single protocol is like trying to use the same map for two different destinations.
The Risks of At-Home Detox for Co-Occurring Dependence
We need to be direct about this: attempting to detox from both alcohol and benzodiazepines at home is one of the most dangerous things you can do. There’s even a term for what happens when people try repeatedly—the “kindling phenomenon.” Each failed attempt at self-detox actually makes the next withdrawal worse, with more severe symptoms and higher seizure risk.
When both substances are involved, the dangers multiply. The increased seizure risk becomes especially concerning because both alcohol and benzos affect your seizure threshold. Removing them incorrectly can trigger seizures that, without medical intervention, can cause lasting damage or death. Respiratory depression remains a threat even during withdrawal—your breathing can slow or stop if the process isn’t carefully managed.
The severe psychological distress that accompanies dual withdrawal goes beyond ordinary anxiety. We’re talking about panic attacks that make you feel like you’re dying, psychosis where reality becomes distorted, and suicidal thoughts that can feel overwhelming. These aren’t symptoms you should face without professional support.
Then there’s the reality of higher relapse rates. The research tells a sobering story: after three years, 62.4% of people who received professional detox were still in remission, compared to only 43.4% who tried to stop on their own. After 16 years, the difference remains stark—60.5% of the “no-help” group relapsed, versus 42.9% of those who got treatment.
We understand the appeal of trying to handle detox at home. It feels private, it seems less expensive, and there’s a certain pride in wanting to do it yourself. But this is one situation where going it alone is a gamble with stakes you can’t afford to lose. A safe, controlled environment in a licensed Florida detox facility provides the round-the-clock medical monitoring that turns a potentially fatal situation into a manageable medical process. Here in Miami, we’ve seen too many people arrive at our doors after dangerous attempts at home detox. We’d much rather see you walk through our doors before you take that risk.
Traditional vs. Modern Approaches to Alcohol Withdrawal
For decades, the medical community has relied on a tried-and-true approach to treating acute alcohol withdrawal: benzodiazepines. These medications work by mimicking alcohol’s calming effect on GABA receptors in the brain, essentially stepping in to prevent the dangerous overactivity that can lead to seizures and delirium tremens. It’s been the gold standard because, frankly, it works.
One of the most important tools in managing alcohol withdrawal is something called the CIWA-Ar scale—the Clinical Institute Withdrawal Assessment for Alcohol, revised. Think of it as a thermometer for withdrawal symptoms. This 10-item scale helps doctors and nurses objectively measure what you’re experiencing and decide when medication is needed. A score under 10 typically means you’re managing okay without medication. Between 10 and 20 suggests you need closer monitoring and possibly treatment. Above 20? That’s when immediate medical intervention becomes critical.
But here’s where things get complicated. While benzodiazepines have saved countless lives during alcohol detox, they’re not without their own challenges. One of the biggest headaches—literally and figuratively—is something we call delirium confusion. When someone is going through severe alcohol withdrawal, they might experience delirium. But benzodiazepines themselves can also cause delirium. For clinicians, it becomes a puzzle: Is this person confused because of the alcohol withdrawal, or because of the medication we’re giving them? Should we increase the dose or back off? It’s not always clear.
There’s another concern that’s particularly relevant for anyone seeking lasting recovery in Miami or throughout Florida: evidence suggests that using benzodiazepines during alcohol detox might actually increase cravings for alcohol down the road. Some studies indicate this approach could lead to a shorter time before someone relapses compared to protocols that minimize benzodiazepine use. That’s a sobering thought when you’re trying to build a foundation for long-term sobriety.
Symptom-Triggered vs. Fixed-Schedule Protocols
When benzodiazepines are used for alcohol withdrawal, there are two main ways to administer them, and the difference between them matters more than you might think.
The fixed-schedule approach is straightforward: you get benzodiazepines at set times throughout the day, regardless of how you’re feeling at that moment. It’s predictable and easy to follow, but it has a significant drawback. You might be feeling relatively comfortable, yet you’re still getting medication you don’t necessarily need. This leads to higher total medication use, longer treatment periods, and a greater risk of over-sedation—that groggy, disconnected feeling that nobody enjoys.
The symptom-triggered approach is smarter and more personalized. Medication is given only when your withdrawal symptoms reach a certain level on that CIWA-Ar scale we mentioned. The results speak for themselves: one study found that patients using this approach took six times less medication and completed treatment in about 20 hours compared to nearly 63 hours for the fixed-schedule group. Even more impressive? More than 60% of patients in the symptom-triggered group didn’t need any benzodiazepines at all.
| Feature | Symptom-Triggered Approach | Fixed-Schedule Approach |
|---|---|---|
| Medication Use | Lower total medication dosage (e.g., 6x less oxazepam) | Higher total medication dosage |
| Treatment Duration | Shorter treatment duration (e.g., 20.0 hours vs 62.7 hours) | Longer treatment duration |
| Oversedation Risk | Lower risk of over-sedation | Higher risk of over-sedation |
| Patient Comfort | Comparable comfort levels | Comparable comfort levels |
| Effectiveness | Safe and effective, with fewer complications | Safe and effective, but potentially less efficient |
| Flexibility | Highly individualized, based on real-time symptoms | Less individualized, doses given regardless of current symptoms |
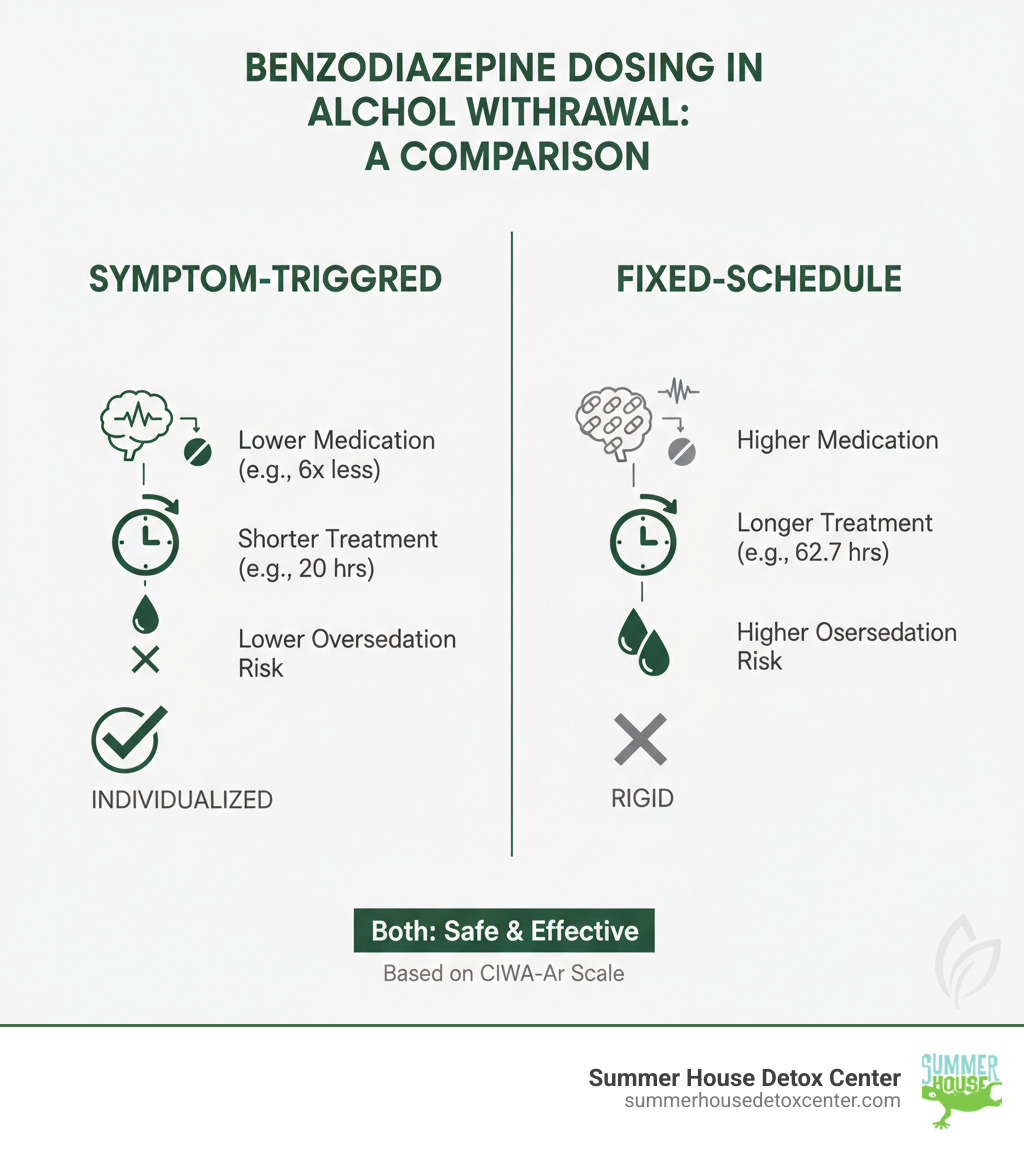
Both approaches are safe and keep patients comfortable, but the symptom-triggered method is more efficient and exposes you to less medication overall. This is especially important for anyone wondering does benzodiazepines detox protocol cover alcohol as well as specialized alternatives—because the answer increasingly involves using less benzodiazepines, not more.
Benzodiazepine-Minimizing Protocols: The Alternatives
The medical field is always evolving, and addiction medicine is no exception. Recognizing the limitations and potential risks of heavy benzodiazepine use, treatment centers—including those serving patients throughout Florida—are now embracing benzodiazepine-minimizing protocols. These modern approaches use alternative medications that can manage withdrawal symptoms just as effectively, sometimes with fewer side effects.

Gabapentin has emerged as a particularly promising option. This medication works comparably to benzodiazepines in managing alcohol withdrawal, but with a crucial advantage: it has a much lower potential for abuse. Studies show it can lead to a faster decline in CIWA scores without extending hospital stays. For someone in recovery, knowing your detox medication won’t create a new dependency is incredibly reassuring.
Valproic acid, an anticonvulsant, has also shown impressive results. It helps stabilize the overactive brain activity that happens during withdrawal and can reduce CIWA scores even more rapidly than benzodiazepines while providing equal symptom control. It’s another tool that helps us move away from the one-size-fits-all benzodiazepine approach.
Clonidine takes a different angle. This medication specifically targets the autonomic hyperactivity you experience during withdrawal—the racing heart, the sweating, the high blood pressure that makes you feel like you’re constantly on edge. When used alongside other medications, clonidine has shown comparable or even superior results in reducing overall withdrawal symptoms compared to benzodiazepines alone.
The real-world impact of these protocols is significant. One study found that implementing a benzodiazepine-minimizing protocol reduced peak 24-hour lorazepam use substantially. Within the protocol group itself, there was a 62% average reduction in benzodiazepine use between the old approach and the new one. That’s a dramatic shift that suggests we can keep people safe and comfortable while significantly reducing their exposure to medications that carry their own risks.
These advances matter especially for anyone dealing with co-occurring alcohol and benzodiazepine dependence. The question does benzodiazepines detox protocol cover alcohol as well as a specialized plan becomes clearer when you understand that modern alcohol detox itself is moving toward less benzodiazepine use, not more. At our Miami facility, we’ve seen how these individualized, benzodiazepine-minimizing approaches can make detox safer and set the stage for better long-term outcomes.
Does a Benzodiazepines Detox Protocol Cover Alcohol as Well As a Specialized Plan?
This brings us back to our central question: does benzodiazepines detox protocol cover alcohol as well as a specialized plan designed specifically for alcohol withdrawal? The answer remains a firm no, and understanding why could be the difference between a safe recovery and a medical crisis.

Think of it this way: you wouldn’t use a marathon training plan to prepare for a 100-meter sprint. They’re both running, sure, but the pacing, intensity, and strategy are completely different. The same principle applies to detoxing from alcohol versus benzodiazepines.
The fundamental issue lies in how quickly each substance needs to be addressed. Benzodiazepine detox demands patience—a slow, methodical taper that gives your brain time to readjust. Alcohol withdrawal, on the other hand, is an emergency that requires immediate, aggressive intervention. Using the wrong approach for either substance can be catastrophic.
How does a benzodiazepines detox protocol cover alcohol as well as other substances?
Yes, there’s cross-tolerance between alcohol and benzodiazepines. They both work on the same GABA receptors in your brain, which is why one can temporarily mask withdrawal symptoms from the other. With chronic use of either substance, these GABA receptors become downregulated—essentially, your brain adjusts to having the substance around and doesn’t function normally without it.
When you stop using, your brain’s excitatory neurotransmitters go into overdrive, like a car with no brakes. This is what causes those dangerous withdrawal symptoms we discussed earlier—the tremors, seizures, and potentially fatal complications.
But here’s the critical point: the speed and intensity of this rebound effect are dramatically different for alcohol and benzodiazepines, which is why addressing GABA receptor downregulation requires completely different strategies.
A benzodiazepine detox protocol is designed for the long haul. We’re talking weeks or even months of gradual tapering, carefully reducing doses by tiny amounts to give your brain time to heal and rebalance. This gentle approach is necessary to prevent severe, protracted withdrawal symptoms and the risk of seizures from tapering too quickly.
A benzo protocol is too slow for acute alcohol withdrawal. If we tried to use this gradual approach for someone withdrawing from alcohol, the results would be disastrous. Alcohol withdrawal doesn’t wait weeks to become dangerous—life-threatening symptoms like seizures and Delirium Tremens can develop within 48 to 72 hours. You need rapid stabilization, not a leisurely taper.
On the flip side, an alcohol protocol is too fast for benzo dependence. Alcohol detox protocols aim for quick stabilization, often wrapping up the acute phase within days to a week. Apply this rushed timeline to someone dependent on benzodiazepines, and you’re asking for trouble—severe withdrawal seizures, intense psychological distress, and a host of other potentially fatal complications.
This is why, for Florida residents dealing with both substances, the necessity of a combined, medically-managed plan custom for Miami and Florida patients cannot be overstated. You need a treatment approach that respects the unique demands of each substance while keeping you safe throughout the entire process.
Can a benzodiazepines detox protocol cover alcohol as well as a dedicated protocol?
The straightforward answer is no—a direct swap is unsafe. It’s like trying to fix a broken bone with cold medicine. The treatment simply doesn’t match the problem.
When you’re dependent on both alcohol and benzodiazepines, a specialized protocol is required that addresses each substance in the right order and at the right pace. We’ve seen this countless times here in Miami, and we’ve learned that there’s no shortcut when it comes to dual dependence.
Here’s how a proper, integrated approach typically works. Initial stabilization from alcohol is always the first priority. Alcohol withdrawal can kill you within days, so this phase is urgent and aggressive. We focus on preventing those immediate life-threatening complications—the seizures, the DTs, the severe cardiovascular stress. This might involve using benzodiazepines as a short-term medication (which is different from treating benzo dependence itself), or it might involve some of those alternative medications we discussed earlier like gabapentin or valproic acid.
Once you’re medically stable and past the acute alcohol withdrawal danger zone, we shift gears. Now comes the subsequent slow taper for benzodiazepines—a completely separate phase that requires patience and precision. This often involves switching you to a long-acting benzodiazepine like diazepam, which allows us to make tiny, controlled reductions over an extended period. We’re talking weeks to months here, carefully monitoring how you respond to each small decrease.
Individualized treatment planning is key for Miami and Florida patients dealing with this complex situation. Your history, your current health, the specific benzodiazepines you’ve been taking, how much alcohol you’ve been consuming—all of these factors shape your treatment plan. There’s no cookie-cutter solution because everyone’s brain chemistry and dependence patterns are unique.
This is exactly why professional care in a facility like ours matters so much. We understand that does benzodiazepines detox protocol cover alcohol as well as a dedicated plan? No, but we know how to create an integrated approach that safely addresses both. We’ve helped countless people in South Florida steer this challenging journey, and we know what it takes to get it right.
Why Professional, Medically Supervised Detox in Miami is Essential
When you’re dealing with dependence on both alcohol and benzodiazepines, you’re facing one of the most complex medical challenges in addiction treatment. This isn’t something you can safely steer alone, and the statistics prove it beyond any doubt.
The numbers tell a compelling story about why professional help matters so much. Research tracking people over many years found that after three years, 62.4% of those who received professional treatment were in remission, compared to just 43.4% of those who tried to quit on their own. That’s nearly a 20-point difference—and it only gets more dramatic over time.
The long-term picture is even more striking. When researchers followed up after 16 years, they found that 60.5% of people in the “no-help” group who had been sober at the three-year mark had relapsed. In contrast, only 42.9% of people who received professional treatment and were sober at three years had relapsed. Professional help essentially cuts your long-term relapse risk nearly in half.
These aren’t just numbers on a page. They represent real people in Miami and throughout Florida who faced the same fears and doubts you might be facing right now. They represent lives saved, families reunited, and futures reclaimed.
The complexity of withdrawing from both alcohol and benzodiazepines simultaneously demands constant medical monitoring. Symptoms can escalate rapidly and unpredictably. What seems manageable at 2 PM can become life-threatening by 8 PM. In a professional detox facility, you have a team watching for these changes 24/7, ready to intervene immediately if complications arise.
There’s also something profound that happens when you’re in a safe, supportive environment specifically designed for healing. You’re not white-knuckling it alone in your bedroom, terrified and isolated. You’re surrounded by people who understand exactly what you’re going through because they’ve either been there themselves or have helped hundreds of others through it.
For Florida residents, accessing quality medical detox has never been more important. The warm, humid climate can actually intensify some withdrawal symptoms like sweating and dehydration, making medical supervision even more crucial. A licensed Florida detox facility understands these regional considerations and can adjust care accordingly.
The Summer House Detox Center Approach
We’ve built Summer House Detox Center around a simple but powerful belief: every person deserves personalized care that treats them with dignity throughout the detox process. When you’re dependent on both alcohol and benzodiazepines, cookie-cutter protocols don’t just fall short—they can be dangerous.
That’s why our Miami facility creates individualized treatment plans that address your specific situation. We start by carefully assessing your history with both substances: how long you’ve been using, what doses, any previous withdrawal attempts, your overall health, and what symptoms you’re already experiencing. This assessment guides everything that follows.
Our experienced staff includes people who understand addiction from the inside out—some are in recovery themselves. They bring not just clinical expertise but genuine empathy and hope. They’ve seen people walk through our doors feeling hopeless and leave with a foundation for lasting recovery. They know the journey intimately.
For co-occurring alcohol and benzodiazepine dependence, we typically follow an integrated approach that addresses the immediate danger first while keeping the bigger picture in mind. We’ll stabilize you from acute alcohol withdrawal with constant medical supervision, managing symptoms as they arise to keep you safe and as comfortable as possible. Once you’re medically stable, we carefully transition to managing your benzodiazepine dependence with the slow, gradual taper it requires.
Throughout this process, you’re never just a patient number. You’re a person with a story, with people who love you, with a life worth fighting for. We see that, and we honor it in everything we do.
Comfort matters to us. Detox is hard enough without feeling like you’re in a cold, clinical environment. Our Miami facility is designed to feel welcoming and peaceful—a place where healing can actually begin.
If you’re in Miami, FL, or anywhere in Florida and you’re struggling with both alcohol and benzodiazepines, you don’t have to figure this out alone. You don’t have to risk the dangers of at-home detox. Does benzodiazepines detox protocol cover alcohol as well as a specialized, integrated plan? No—and that’s exactly why you need professional care that understands the difference.
We’re here to provide that first crucial step toward recovery, with the medical expertise and compassionate support you deserve.


