Making the Switch: Your Path to Greater Freedom
Detoxing from methadone to suboxone is a medical transition that many people consider to improve their quality of life and treatment flexibility. This process requires careful medical supervision but can offer significant benefits including fewer clinic visits, reduced stigma, and greater personal freedom.
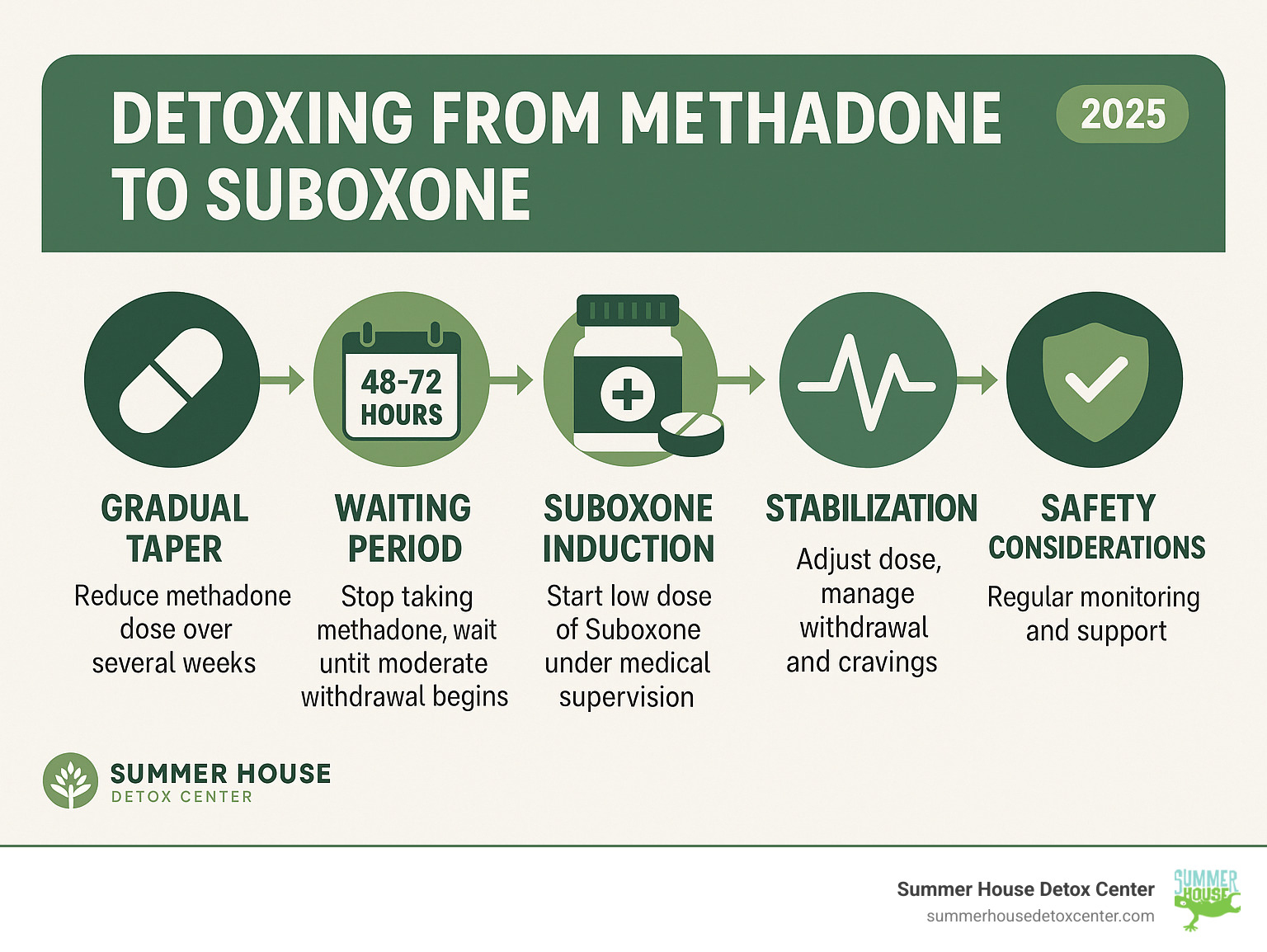
Key Steps for Methadone to Suboxone Transition:
- Medical Evaluation – Your doctor assesses your current methadone dose and overall health
- Gradual Taper – Slowly reduce methadone to 30-40mg daily over several weeks
- Waiting Period – Stop methadone for 48-72 hours to avoid precipitated withdrawal
- Suboxone Induction – Begin with low doses under medical supervision
- Stabilization – Adjust dosage to manage withdrawal and cravings effectively
The transition isn’t just about switching medications – it’s about finding a treatment approach that fits better with your life goals and circumstances. Many people make this switch successfully, but the process requires patience, medical guidance, and often inpatient support to ensure safety and comfort.
As one patient shared in research studies, the fear of transitioning can be overwhelming, but with proper medical supervision, the switch can lead to feeling “normal” again and having more freedom in daily life.
Whether you’re tired of daily clinic visits, experiencing side effects from methadone, or simply want more flexibility in your recovery journey, understanding this transition process is the first step toward making an informed decision about your treatment.
Handy detoxing from methadone to suboxone terms:
Why Transition from Methadone to Suboxone?
Imagine trading daily trips to a clinic for the freedom of managing your medication from home. That’s a significant reason why many individuals choose to transition from methadone to Suboxone. While methadone has long been a cornerstone of opioid use disorder (OUD) treatment, Suboxone often offers a lifestyle that aligns more closely with long-term recovery goals.
Our patients often tell us they seek this transition for several compelling reasons:
- Less Stigma and Increased Privacy: Methadone treatment, often requiring daily clinic visits, can carry a heavy social stigma. Suboxone, which can be prescribed by many doctors and picked up at a regular pharmacy, offers a more discreet treatment experience.
- Fewer Clinic Visits: For those working, attending school, or with family responsibilities, daily methadone clinic visits can be a huge logistical burden. Suboxone allows for much greater flexibility, often with weekly or even monthly prescriptions.
- Improved Quality of Life: Patients report feeling “normal” on Suboxone, contrasting with a “heavy feeling” some experience on methadone. This can translate to better overall well-being and a greater ability to engage in daily life.
- Improved Safety Profile: Suboxone has a “ceiling effect” on respiratory depression, which means that beyond a certain dose, further increases do not significantly improve the risk of slowed breathing, making overdose less likely compared to full opioid agonists like methadone.
- Medication Access: While methadone is tightly regulated and dispensed only at specialized clinics, Suboxone (buprenorphine) offers broader access, as more healthcare providers can prescribe it. This increased accessibility can be a game-changer for many. Medication Access can greatly simplify a patient’s treatment journey.
Understanding Methadone
Methadone is a full opioid agonist used to treat OUD since the 1960s. It fully activates opioid receptors to alleviate withdrawal and cravings without a “high.” As a Schedule II drug, it has a higher potential for abuse and is dispensed only at specialized clinics, often requiring daily visits. Its long duration of action is beneficial for managing cravings but can also lead to severe, prolonged withdrawal if stopped abruptly. Long-term use can be associated with side effects like QTc prolongation, a heart rhythm issue. For more detailed information, you can refer to the Methadone monograph.
Understanding Suboxone
Suboxone is a combination of buprenorphine (a partial opioid agonist) and naloxone (an opioid antagonist). Buprenorphine partially activates opioid receptors to reduce cravings and withdrawal, but with a “ceiling effect” that lowers the risk of overdose. Naloxone is included to deter misuse; it becomes active if the drug is injected, triggering withdrawal. As a Schedule III drug, Suboxone has a lower abuse potential than methadone and offers more flexibility. It can be prescribed by certified doctors and filled at regular pharmacies, making it an attractive and convenient option for many in recovery.
[TABLE] Comparing Methadone and Suboxone
To help you visualize the key differences, here’s a side-by-side comparison of methadone and Suboxone:
| Feature | Methadone | Suboxone (Buprenorphine/Naloxone) |
|---|---|---|
| Mechanism of Action | Full opioid agonist (fully activates receptors) | Partial opioid agonist (partially activates receptors) |
| Controlled Substance Status | Schedule II (higher abuse potential) | Schedule III (lower abuse potential) |
| Dispensing Regulations | Highly restricted, dispensed only at specialized OTP clinics | Can be prescribed by certified doctors and filled at regular pharmacies |
| Overdose Risk | Higher risk of respiratory depression and overdose (no ceiling effect) | Lower risk of respiratory depression and overdose (ceiling effect) |
| Primary Side Effects | Constipation, drowsiness, sweating, QTc prolongation, sexual problems | Headache, nausea, weakness, constipation, drowsiness, sexual problems |
| Withdrawal Severity | Generally more severe and prolonged | Generally less severe and shorter duration (if tapered) |
| Convenience | Requires daily clinic visits (often supervised dosing) | Take-home doses, less frequent clinic visits possible |
| Stigma | Often associated with higher stigma | Generally perceived with less stigma |
The Critical Risk: Understanding Precipitated Withdrawal
When you’re considering detoxing from methadone to suboxone, there’s one really important step we need to talk about, and it’s called precipitated withdrawal. This isn’t just any withdrawal; it’s a sudden, super-intense experience that can happen if Suboxone is given too soon after you’ve been taking a full opioid like methadone. It’s like hitting a fast-forward button on discomfort, and we want to help you avoid it at all costs.
So, why does this happen? It all comes down to how these medications work in your body:
- Buprenorphine’s Strong Grip: The main ingredient in Suboxone, buprenorphine, is super “sticky” when it comes to attaching to the opioid receptors in your brain. Think of it like a very strong magnet.
- Kicking Methadone Out: If you still have methadone (which is also attached to those receptors) in your system when Suboxone is introduced, the buprenorphine will quickly push the methadone off those receptors. It essentially “wins” the spot.
- Sudden Shock to Your System: Because buprenorphine only partially activates these receptors, and because it displaces the methadone so quickly, your body suddenly experiences a big drop in opioid activity. This abrupt change triggers an immediate and severe onset of withdrawal symptoms. Many describe it as far worse than natural withdrawal, feeling “nearly intolerable.”
This is why waiting is crucial when detoxing from methadone to suboxone. We need to give your body enough time for the methadone to naturally clear out of your system. Methadone has a long half-life, meaning it takes a while to leave your body. You’ll typically need to wait at least 48 to 72 hours after your last methadone dose, and sometimes even longer, depending on your individual body and the dose you were on.
During this waiting period, you’ll likely start to feel some withdrawal symptoms. This is actually a good sign! It means your body is ready for the Suboxone. To make sure the timing is just right, medical professionals use tools like the Clinical Opiate Withdrawal Scale (COWS). This scale helps us objectively measure your symptoms. A score of 17 or higher on the COWS scale often indicates you are in enough withdrawal to begin Suboxone safely. This careful monitoring is a cornerstone of our approach at Summer House Detox Center, ensuring your transition is as comfortable and safe as possible.
A Guide to Detoxing from Methadone to Suboxone
Starting on the journey of detoxing from methadone to suboxone can feel daunting, but with the right guidance and support, it’s a transition that can significantly improve your recovery. There are two primary methods for this switch, each with its own considerations, and medical supervision is absolutely essential for both. At Summer House Detox Center, we believe in crafting individualized treatment plans because we know that every person’s path to recovery is unique.
For those considering this important step, it’s reassuring to know that effective Medications for Substance Use Disorders are available, and the transition can be managed safely.
The Standard Approach to Detoxing from Methadone to Suboxone
This method prioritizes a gradual, controlled process. Our goal is always to minimize discomfort and the critical risk of precipitated withdrawal we discussed earlier.
First, we begin with a gradual methadone taper. This involves slowly reducing your methadone dose over several weeks. Experts recommend tapering to about 30-40 mg daily and holding at that dose for at least a week. Reducing the dose by no more than 5-10% per week allows your body to adjust gently.
Next comes a crucial waiting period. Once your methadone dose is low enough, you’ll stop taking it entirely for 36-72 hours (sometimes longer). This “washout” period is vital to ensure enough methadone has cleared your system before we introduce Suboxone.
This brings us to monitoring for withdrawal. During this time, you will experience withdrawal, which is a necessary sign that your body is ready. Our medical team will closely watch your symptoms using tools like the COWS scale (Clinical Opiate Withdrawal Scale). It’s crucial that you are in moderate to severe withdrawal (typically a COWS score of 17 or higher) before we give you the first dose of Suboxone. This ensures the buprenorphine in Suboxone can bind effectively to your receptors without causing that harsh precipitated withdrawal. For more comprehensive guidance, you can consult Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings.
Once you’re in the right state of withdrawal, we begin buprenorphine induction. This starts with a very low initial dose of Suboxone (e.g., 2 mg), given under close medical supervision to monitor your response and ensure comfort.
Finally, we move to titration to a stable dose. Over the next few days, your Suboxone dosage is gradually increased until we find the dose that effectively manages your cravings and withdrawal symptoms. This process typically takes about two days.
Rapid Detoxing from Methadone to Suboxone: The Naltrexone Method
For some in an inpatient setting, a rapid transition using naltrexone may be an option. This method uses naltrexone-induced withdrawal; as an opioid antagonist, naltrexone rapidly blocks opioid receptors, forcing an acute withdrawal state. Because this process is so intense, it requires a highly supervised medical environment. You can expect rapid symptom onset, often within 45 minutes, after which buprenorphine is immediately administered as a “rescue” to alleviate the severe symptoms. The main benefit is speed, as it can shorten the transition time significantly. However, the risks are considerable. Studies show a high percentage (96%) of individuals experience agitation, and about 1% suffer severe adverse events like heart attack or seizure. This method underscores the necessity of expert medical supervision in a specialized facility.
Common Withdrawal Symptoms and Timeline
Regardless of the method chosen, experiencing some withdrawal symptoms is a normal part of the transition. Our goal is always to make this process as comfortable as possible for you.
Here’s a list of common withdrawal symptoms you might experience:
- Nausea and vomiting
- Diarrhea and digestive distress
- Muscle aches and cramps
- Headaches
- Insomnia
- Lethargy and fatigue
- Anxiety and irritability
- Depression and mood swings
- Intense drug cravings
- Fever, chills, and sweating
- Difficulty concentrating
Understanding the Withdrawal Timeline:
- Methadone Withdrawal: Due to its long half-life, symptoms can begin within 48 hours and last up to 20 days or more.
- Suboxone Withdrawal: If tapered, physical symptoms typically start within 24 hours, peak in the first 72 hours, and last up to 10 days. Psychological symptoms can linger for months.
We understand that dealing with these symptoms can be challenging. That’s why we emphasize a comfortable, medically supervised detox experience. For more information about our approach to managing withdrawal symptoms, explore our comfortable detox services.
The Importance of Professional Support During Transition
Making the switch from methadone to Suboxone is a significant step forward on your recovery journey. But here’s the honest truth: it’s a journey you should never try to walk alone. Professional support isn’t just helpful; it’s absolutely vital for your safety, comfort, and long-term success. Think of it as having your own expert guide for a challenging, but incredibly rewarding, trip.

Medical Supervision and Safety
At Summer House Detox Center, our medical team provides 24/7 monitoring throughout your transition. Why is this so important when detoxing from methadone to suboxone? Because this continuous oversight allows us to ensure your safety every step of the way. We keep a close eye on your vital signs and overall well-being, ready to step in if any little hiccup arises.
Our team is dedicated to managing withdrawal symptoms, using a combination of medications and supportive care to make sure you’re as comfortable as possible. We understand that withdrawal can be tough, and our goal is to ease that discomfort. Plus, the Suboxone induction process needs careful handling. Our team will adjust your medication dosage in real-time, based on how you’re feeling, ensuring you get exactly the right amount at the right time. This precise care helps prevent complications like severe dehydration or electrolyte imbalances that can sometimes pop up during withdrawal.
This kind of personalized medical care is especially crucial if you have other health conditions or are on a higher methadone dose. While many people transition smoothly, even those on lower doses benefit immensely from expert guidance.
So, who is often an ideal candidate for this transition? Generally, it’s someone who is seeking more flexibility in their treatment, perhaps tired of daily clinic visits. It could be someone experiencing significant side effects from methadone, like really bad constipation or excessive sweating. Or maybe you simply desire a less restrictive treatment environment and have a stable support system with a strong motivation for change.
However, it’s important to know that this path isn’t for everyone, especially the more rapid transition methods. If you have serious, unstable medical conditions, like severe heart, lung, or neurological issues, a rapid transition might not be safe. It’s always best to have an open and honest conversation about your full medical history with your care team. For more general insights into addiction and recovery, explore Substance Abuse and Addiction Blogs.
Psychosocial Support and Long-Term Recovery
Medication-assisted treatment (MAT), which includes the process of detoxing from methadone to suboxone, works best when it’s part of a bigger plan that looks at you as a whole person. At Summer House Detox Center, we go beyond just managing medication. We truly believe in supporting your entire well-being.
That’s why we emphasize individual therapy. These one-on-one sessions give you a safe space to explore why you might have turned to substances, learn new ways to cope, and address any other mental health concerns like anxiety or depression. There’s also group counseling, where you can share experiences with others who truly understand your journey. It builds a sense of community, makes you feel less alone, and helps everyone support each other. Many people also find strength and guidance in programs like 12-Step treatment, which focuses on personal growth and lasting sobriety.
We’ll also help you develop strong coping strategies and relapse prevention skills. This means learning to spot triggers and finding healthy ways to manage cravings and stress without turning back to substance use. It’s about equipping you with practical tools for navigating life’s challenges. And building a strong, positive support network is key. Recovery is always easier and more fulfilling when you have encouraging people by your side.
Many experts agree that therapy is truly the key to long-term sobriety. Without addressing the thoughts, feelings, and behaviors behind addiction, staying sober can be incredibly tough. Our therapeutic treatment plan is designed to give you all the tools and resilience you need for a lasting, joyful recovery.
Frequently Asked Questions about the Methadone to Suboxone Transition
When you’re considering detoxing from methadone to suboxone, it’s natural to have a lot of questions. This is a big step, and we want you to feel fully informed and comfortable. Here, we’ll walk through some of the most common things people ask us, providing clear and helpful answers.
Can Suboxone itself be addictive?
This is an important question. Yes, Suboxone has the potential for physical dependence because its active ingredient, buprenorphine, is an opioid. This means your body can get used to it, and stopping suddenly can cause withdrawal. That’s why it’s a Schedule III controlled substance. However, buprenorphine is a ‘partial’ agonist, which gives it a lower risk of abuse and a ‘ceiling effect’ compared to full opioids like methadone. The naloxone in Suboxone also helps deter misuse. The key to using it safely and effectively is to follow your doctor’s instructions precisely. For more on OUD, you can consult resources on Opioid Use Disorder (OUD).
What are the potential side effects of methadone and Suboxone?
Like any medication, both can have side effects. Our medical team works to manage these to keep you comfortable. Many side effects are similar for both:
- Feeling constipated
- Nausea or vomiting
- Feeling a bit dizzy
- Having trouble concentrating
- Feeling drowsy
- Sometimes, even shallow breathing
- And for some, sexual problems
Methadone has a specific risk of a heart rhythm issue called QTc prolongation and can cause a ‘heavy’ feeling. For more details, see the Methadone side effects information.
Suboxone may cause headache, weakness, or mouth irritation where the film dissolves. Our team can help manage these, often by adjusting your dose. Refer to the Suboxone side effects information for more.
Can you take methadone and Suboxone together?
This is a firm no; taking them together is dangerous and strongly discouraged. The main reason is the high risk of ‘precipitated withdrawal.’ The buprenorphine in Suboxone has a stronger bond to your brain’s opioid receptors than methadone. If you take Suboxone while methadone is still in your system, the buprenorphine will rapidly kick the methadone off the receptors, triggering a sudden and severe withdrawal state. The manufacturer of Suboxone recommends against it. The only exception is a highly complex ‘microdosing’ protocol (the Bernese method) performed under constant, expert medical supervision in a specialized facility like ours. It is not a standard approach and should never be attempted otherwise.
Begin Your Transition to a Freer Life
You’ve learned about the transition from methadone to Suboxone—a significant step toward a freer, more flexible life in recovery. We’ve covered the reasons for switching and the careful steps required to do so safely.
The idea of making this change can feel intimidating, especially with the risks like precipitated withdrawal. But here’s the good news: this transition is achievable and can profoundly improve your quality of life. Imagine saying goodbye to those daily clinic visits and embracing a sense of normalcy you’ve been longing for.
However, as we’ve learned, safety is paramount. The precise steps of tapering, that crucial waiting period, and the careful timing of Suboxone induction demand professional expertise.
That’s where we come in. At Summer House Detox Center, our medical team creates personalized plans just for you. We understand the fears, the challenges, and the hopes you bring with you. Our goal is to provide 24/7 medical supervision, ensuring your comfort and dignity every step of the way. With a team that includes staff members who’ve walked similar paths, you’ll find genuine comfort measures and comprehensive psychosocial support to steer this process successfully.
Your journey toward a healthier, more independent life isn’t just a dream – it’s truly within reach. If you’re ready to explore this important switch with confidence and compassionate care, please don’t hesitate. Contact us today to learn about our medically supervised detox programs. We’re here to help you take that courageous next step.

