Why Understanding Opiate Withdrawal is Critical for Your Recovery
Coping with opiate withdrawal can feel overwhelming, but understanding the process makes it manageable with the right support and medical care.
Quick Answer for Managing Withdrawal Symptoms:
- Seek medical supervision – Never attempt withdrawal alone due to serious risks
- Stay hydrated – Drink 2-3 liters of water daily to replace fluids lost through sweating
- Use comfort measures – Hot baths, loose clothing, heating pads for muscle aches
- Take approved medications – OTC options like ibuprofen for pain (with doctor approval)
- Get emotional support – Friends, family, or professional counseling
- Prepare your environment – Stock up on electrolyte drinks, bland foods, and distractions
If you’re struggling with opioid dependence in Miami or anywhere in Florida, you’re not alone. Research shows that withdrawal symptoms typically start within 6-12 hours for short-acting opioids like heroin and within 12-48 hours for long-acting ones like methadone.
The reality is stark but hopeful: While withdrawal can feel like a severe flu, it’s not life-threatening like alcohol withdrawal. Physical symptoms usually last only a few days, though cravings and emotional symptoms can persist longer.
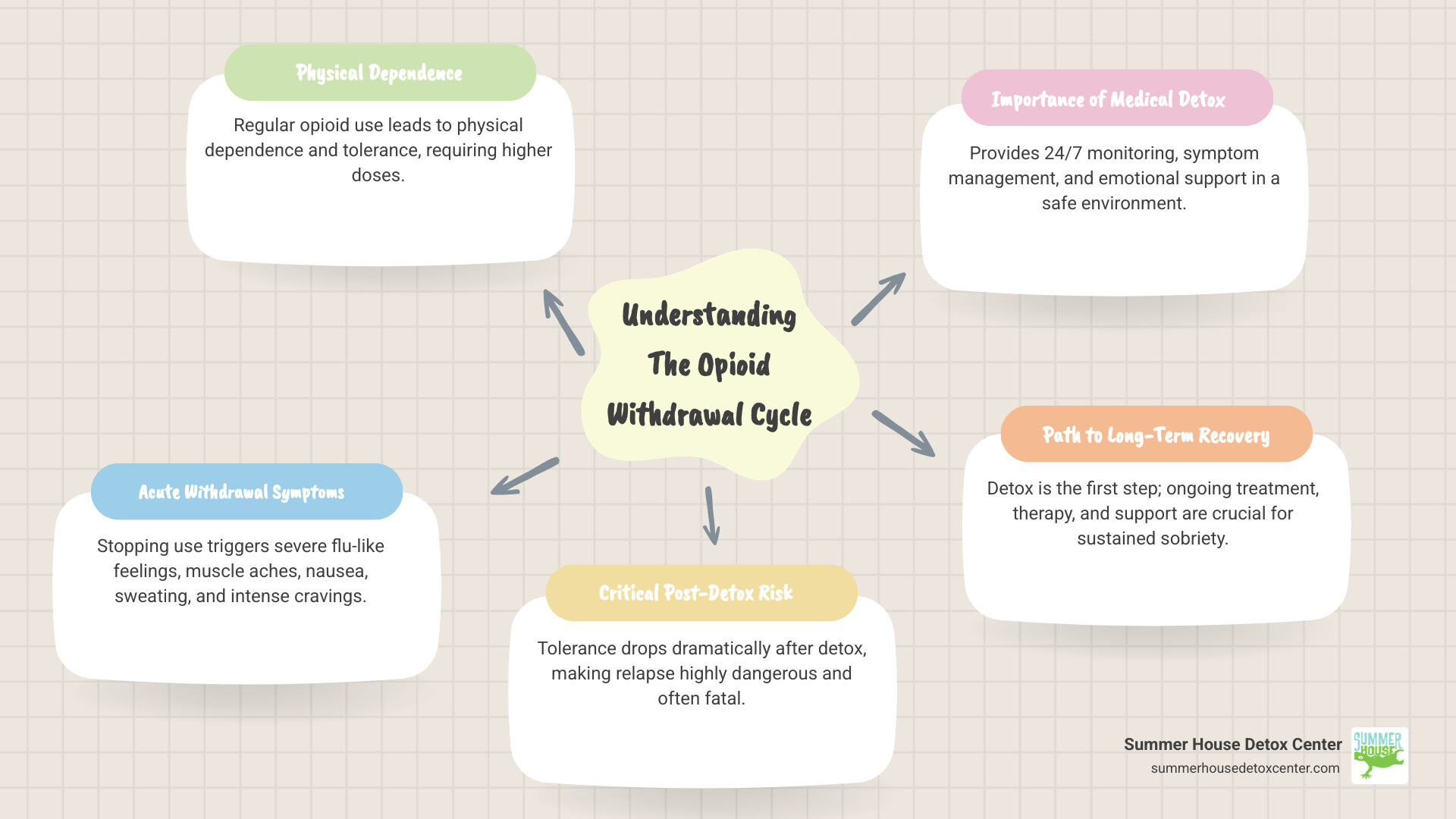
Here’s what makes withdrawal so challenging – and why professional help matters. When you stop using opioids after regular use, your body needs time to readjust. Most people experience muscle aches, nausea, sweating, and intense cravings during this process.
The biggest risk isn’t the withdrawal itself – it’s what happens after. Most opiate overdose deaths occur in people who have just detoxed because their tolerance drops dramatically. This is why withdrawal management without ongoing treatment isn’t recommended.
Florida residents have access to quality medical detox programs that can make this process safer and more comfortable. Medical supervision provides 24/7 monitoring, symptom management medications, and emotional support during your most vulnerable time.
Handy coping with opiate withdrawal terms:
- opiate withdrawal symptoms
- does gabapentin help with opiate withdrawal symptoms
- herbal remedies for opiate withdrawal symptoms
Understanding Opiate Withdrawal: Symptoms and Timeline
When your body gets used to having opioids around, it starts depending on them to feel normal. This is called physical dependence, and it’s different from addiction – it can happen to anyone who takes opioids regularly, even when following a doctor’s prescription.
Over time, your body also builds up tolerance. This means you need more of the drug to get the same relief you used to get from a smaller amount. It’s your body’s way of adapting, but it sets the stage for withdrawal when you stop.
Coping with opiate withdrawal starts with understanding what you’re facing. When you stop using opioids, your body essentially throws a tantrum because it doesn’t know how to function without them anymore. The good news? This is temporary, and knowing what to expect can make it much less scary.
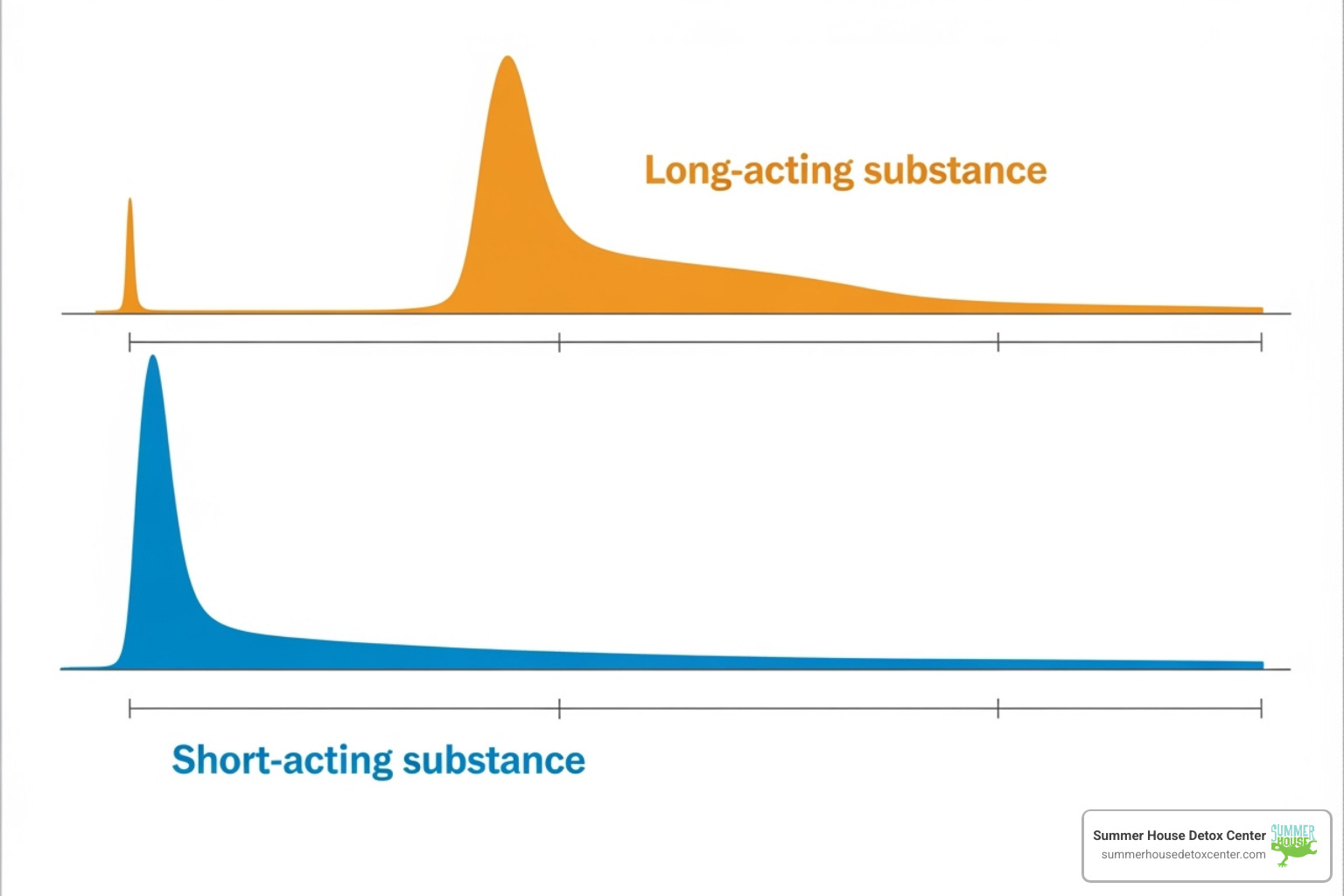
The timeline for withdrawal depends heavily on the drug’s half-life – basically, how long it takes your body to clear out half of the drug. Understanding these Opiate Withdrawal Symptoms and their patterns helps you prepare for what’s ahead.
Early and Late Stage Symptoms
Think of withdrawal symptoms like a wave that builds up and then crashes down. Early symptoms usually show up first and feel a lot like getting hit with the worst flu of your life.
You might notice muscle aches that make you feel like you’ve run a marathon, along with anxiety that seems to come out of nowhere. Your eyes might start tearing up more than usual, and you’ll probably find yourself yawning constantly – even when you’re not tired.
Flu-like feelings dominate this stage. You’ll likely experience excessive sweating, a runny nose, and restlessness that makes it impossible to get comfortable anywhere.
As withdrawal progresses, late symptoms kick in and tend to hit your digestive system hard. Nausea and vomiting can make it difficult to keep anything down, while diarrhea and abdominal cramping add to the misery.
You might notice your skin getting goosebumps frequently – this is actually where the phrase “cold turkey” comes from. Your heart rate speeds up, your pupils get bigger, and you might feel like your body temperature is all over the place.
Here’s something important to remember: unlike withdrawal from alcohol or some other substances, opiate withdrawal won’t cause seizures or put your life in immediate danger. But it’s still incredibly uncomfortable, which is why medical support makes such a difference.
For more detailed information about what you might experience, check out What are the Symptoms of Opiate Withdrawal?
Withdrawal Timelines: Short-Acting vs. Long-Acting Opioids
The type of opioid you’ve been using makes a huge difference in your withdrawal timeline. It’s like the difference between ripping off a bandage quickly versus peeling it off slowly.
Short-acting opioids like heroin and many prescription painkillers (think oxycodone or hydrocodone) leave your system faster. This means withdrawal hits you sooner but doesn’t last as long.
With short-acting drugs, symptoms typically start within 6-12 hours after your last dose. They usually peak around 24-48 hours – this is when you’ll feel the worst. The good news is that physical symptoms generally start improving after 3-5 days, though you might still feel some effects for up to two weeks.
Long-acting opioids like methadone are a different story entirely. These drugs stick around in your system much longer, so withdrawal takes longer to start but also lasts much longer.
With long-acting opioids, you might not feel withdrawal symptoms for 2-4 days after stopping. When they do start, the acute phase can last 10 days or even longer. Some people continue feeling unwell and experiencing cravings for months.
This is why the question How Long Does it Take to Withdraw from Opiates? doesn’t have a simple answer – it really depends on what you’ve been taking and for how long.
Understanding your specific timeline helps you prepare mentally and practically for the journey ahead. It also helps medical professionals in Florida create the right treatment plan for your situation.
The Dangers of Quitting Alone vs. The Safety of Medical Detox
The thought of going through withdrawal might make you consider just coping with opiate withdrawal on your own – after all, how hard could it be? Unfortunately, this thinking can be dangerous and even deadly. While opioid withdrawal itself won’t kill you like alcohol withdrawal might, the complications and risks that come with going it alone create serious hazards that many people don’t see coming.
The biggest danger isn’t actually the withdrawal symptoms themselves. It’s what happens after you make it through those brutal few days. Your tolerance drops dramatically during withdrawal, but your brain doesn’t forget how much you used to take. If you relapse – and most people who try to quit alone do – taking your “normal” dose can easily lead to an overdose. This is why most opiate overdose deaths happen to people who recently went through detox.
Why “Cold Turkey” Is So Risky
Going “cold turkey” means facing withdrawal symptoms at their absolute worst, with no medical support to help you through. The intense cravings and severe discomfort can feel overwhelming – imagine the worst flu you’ve ever had, multiplied by ten, with crushing anxiety and depression on top.
The psychological distress hits just as hard as the physical pain. Without medical support to manage your symptoms, thinking clearly becomes nearly impossible. You’re dealing with severe anxiety, depression, and irritability while your body feels like it’s falling apart. This combination traps many people in a cycle where using again feels like the only escape.
Dehydration and aspiration pneumonia pose real medical dangers during unmanaged withdrawal. All that sweating, vomiting, and diarrhea can lead to dangerous fluid loss and electrolyte imbalances. If you’re vomiting severely, you risk inhaling vomit into your lungs, which can cause aspiration pneumonia.
The statistics on high relapse rates for people who try to quit alone are sobering. Most people simply can’t tolerate the intensity of unmanaged symptoms and return to using just to make the pain stop. Without proper support and a transition plan to ongoing treatment, even those who make it through withdrawal often relapse within days or weeks.
For more details on these serious risks, check out What are the Risks of Quitting Opiates Cold Turkey?.
The Benefits of Medically Supervised Detox in Florida
Here in Florida, especially at Summer House Detox Center in Miami, we’ve seen how different the withdrawal experience can be with proper medical supervision. Coping with opiate withdrawal becomes manageable when you have the right support system in place.
24/7 medical monitoring means someone is always watching out for you. Our medical staff continuously checks your vital signs, monitors your symptoms, and adjusts your care plan in real-time. If complications arise – like dangerous dehydration or blood pressure changes – we catch them immediately.
Symptom management through carefully selected medications makes withdrawal significantly more comfortable. We can reduce the muscle aches, control nausea and vomiting, help with sleep, and ease anxiety. You’re still going through withdrawal, but you don’t have to suffer through it.
The safe environment at our facility removes you from all the triggers and stresses that might push you toward using again. Our staff understands exactly what you’re experiencing because many of them have walked this path themselves. That kind of empathy and understanding makes a huge difference when you’re feeling hopeless.
Nutritional support and emotional care work together to help your body and mind heal. We make sure you stay properly hydrated with the right balance of electrolytes, and we provide nourishing meals even when you don’t feel like eating. Our team offers compassionate emotional support to help you steer the anxiety, depression, and other psychological challenges.
Most importantly, medically supervised detox provides a transition to ongoing treatment. Detox alone isn’t treatment – it’s just the first step. We help you move smoothly into medication-assisted treatment, counseling, and therapy programs that give you the best chance at long-term recovery.
If you’re wondering whether medical detox is right for your situation, learn more about Who Needs Opiate Detox in Florida?. Miami residents have access to quality care that can make this challenging process safer and more successful.
Medical Approaches for Coping with Opiate Withdrawal
When you’re facing the challenge of coping with opiate withdrawal, having the right medical support can transform what feels like an impossible situation into a manageable healing process. At Summer House Detox Center in Miami, we’ve seen how proper medical care makes all the difference between suffering through withdrawal alone and moving through it with comfort and dignity.

Medication-Assisted Treatment (MAT) forms the backbone of our approach to withdrawal management. Think of it as giving your body the support it needs while it learns to function without opioids again. Rather than white-knuckling through intense symptoms, MAT uses specific medications to ease your discomfort, reduce those overwhelming cravings, and significantly lower your risk of relapse.
The goal isn’t just to get you through withdrawal – it’s to make the process as smooth and comfortable as possible so you can focus your energy on healing and preparing for the next phase of your recovery journey. This medical approach is a cornerstone of what we offer at our Opiate Detox Center.
The Role of Medications in Easing Withdrawal
Several proven medications can dramatically improve your withdrawal experience. Your doctor will choose the right combination based on your specific situation – what type of opioid you’ve been using, how severe your symptoms are, and your individual medical needs.
| Medication | Purpose | How it Works | Considerations |
|---|---|---|---|
| Methadone | Long-term maintenance and withdrawal management | Acts on the same brain receptors as other opioids but more slowly and steadily, preventing withdrawal while blocking euphoric effects | Requires daily clinic visits and careful monitoring due to potential for overdose |
| Buprenorphine | Withdrawal management and maintenance | Partially activates opioid receptors, providing enough stimulation to prevent withdrawal without causing a high | Safer than methadone with lower overdose risk; can be prescribed in office settings |
| Clonidine | Symptom relief | Originally a blood pressure medication that helps reduce anxiety, sweating, muscle aches, and other physical symptoms | Doesn’t address cravings but very effective for physical discomfort |
Methadone has been helping people recover from opioid addiction for decades. It works by occupying the same brain receptors that other opioids target, but it does so in a controlled, steady way that prevents withdrawal symptoms without causing the highs and lows of street drugs.
Buprenorphine, often given as Suboxone (which includes naloxone to prevent misuse), offers a gentler approach. It’s what doctors call a “partial agonist” – it activates your opioid receptors just enough to keep withdrawal at bay but has a “ceiling effect” that makes overdose much less likely.
Clonidine tackles the physical misery of withdrawal head-on. While it won’t eliminate cravings, it can significantly reduce the sweating, anxiety, muscle aches, and restlessness that make withdrawal so unbearable. Lofexidine works similarly but is specifically FDA-approved for opioid withdrawal.
We also use adjunctive medications – additional medicines that target specific symptoms like nausea, diarrhea, or insomnia. These might include anti-nausea medications, sleep aids, or anti-anxiety medicines used carefully and for short periods.
Understanding Which Medications Are Used in Opiate Detox? helps you feel more prepared and less anxious about the process.
Assessing Withdrawal Severity: The COWS Scale
One of the tools that helps our medical team provide the best care is the Clinical Opiate Withdrawal Scale (COWS). This isn’t as intimidating as it sounds – it’s simply a way for doctors and nurses to objectively measure how you’re feeling during withdrawal.
The COWS scale looks at 11 physical signs including your pupil size, heart rate, tremors, sweating, restlessness, and other symptoms. By scoring these on a scale, your medical team can track whether you’re improving or if you need additional medication adjustments.
This objective measurement system means your care isn’t based on guesswork. Instead of just asking “How do you feel?” (which can be hard to answer when everything hurts), the COWS scale gives your medical team concrete data to guide your treatment. If your score shows increasing distress, they can adjust your medications immediately. If it shows you’re improving, they know the current approach is working.
For anyone in Miami or throughout Florida who’s been putting off getting help because they’re afraid of withdrawal, remember this: modern medical approaches to coping with opiate withdrawal have come a long way. You don’t have to suffer through this alone, and you don’t have to endure unnecessary pain. With the right medical support, withdrawal can be the bridge to your new life rather than a wall that stops you from getting there.
