Understanding Light Opiate Withdrawal Symptoms: The First Step to Recovery
Light opiate withdrawal symptoms represent the milder end of the spectrum that individuals experience when they reduce or stop using opioids after a physical dependence has formed. This dependence isn’t a moral failing or a sign of weakness; it’s a predictable physiological response where the body adapts to the consistent presence of an opioid. When that substance is removed, the body needs time to readjust, leading to a series of withdrawal symptoms. While these symptoms are uncomfortable, they are generally manageable and significantly less severe than what is seen in full-blown, acute withdrawal.
Understanding where your symptoms fall on this spectrum is the crucial first step toward making informed and safe decisions about your recovery. Light withdrawal is most common in individuals who have used lower doses of opioids, have been using them for a shorter duration, or are carefully tapering their dosage under medical supervision.
Common light opiate withdrawal symptoms include:
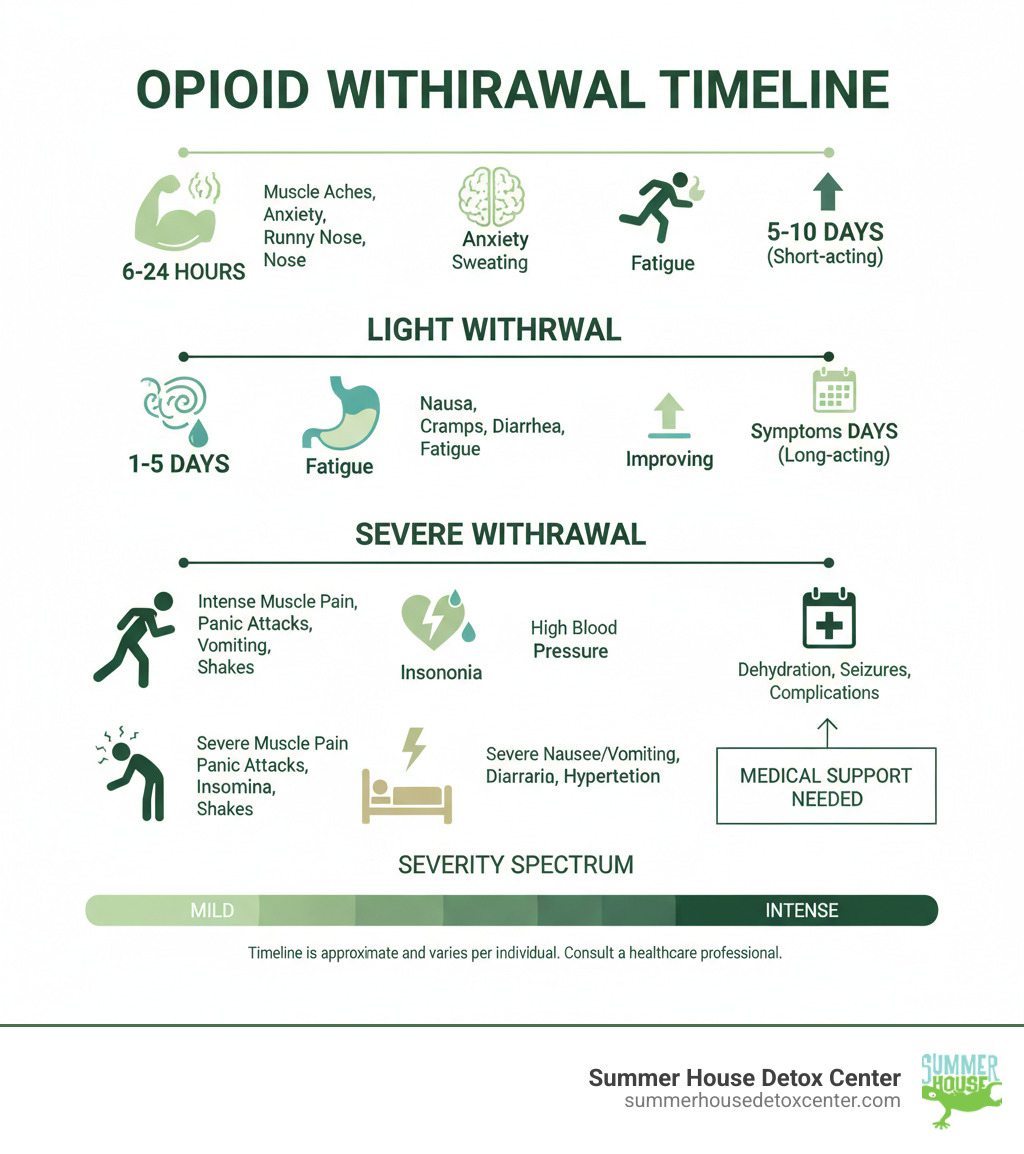
- Early symptoms (developing within 6-24 hours): These often begin subtly. You might feel a deep ache in your muscles and bones, similar to the onset of a bad flu. A persistent sense of anxiety or edginess can set in, making it hard to relax. Physical signs often include a runny nose, excessive tearing, frequent yawning, and sweating even when you don’t feel hot. Restlessness can make it difficult to sit still or get comfortable.
- Later symptoms (peaking around 1-5 days): As withdrawal progresses, gastrointestinal issues like mild nausea, stomach cramps, and diarrhea may appear. You might notice goosebumps on your skin, a classic sign that gives “cold turkey” its name. A profound sense of fatigue and lethargy can set in, making even simple tasks feel exhausting. All the while, psychological and physical drug cravings can become more persistent, creating a significant mental hurdle.
- Duration: The timeline for these symptoms varies based on the type of opioid used. For short-acting opioids like heroin, fentanyl, or immediate-release prescription painkillers, symptoms typically last for 4-10 days. For long-acting opioids such as methadone or extended-release formulations, the withdrawal process is more drawn out, often lasting 10-20 days or longer.
- Intensity: The overall experience is often described as “flu-like.” However, this comparison can be misleading, as it doesn’t account for the intense psychological components of anxiety, depression, and cravings that accompany the physical discomfort. While not considered life-threatening, the experience is draining and challenging to endure without support.
Research confirms that withdrawal symptoms can begin as early as 6 to 16 hours after the last dose, typically peaking within the first few days. It’s essential to remember that while these symptoms can feel overwhelming, they are a sign that your body is beginning its natural healing process, recalibrating its chemistry to function without the presence of opioids.
For residents of Miami and across Florida, where opioid misuse remains a significant public health concern, recognizing these early warning signs is critical. It allows you to seek appropriate support before symptoms potentially escalate into a more severe and dangerous state. Whether you’re struggling with prescription painkillers obtained legally or illicit substances, understanding your body’s signals and the withdrawal timeline empowers you to take the next, safer step on your recovery journey.
Understanding the Spectrum: Mild vs. Severe Opioid Withdrawal
When you’re facing opioid withdrawal, it’s crucial to understand that the experience is not one-size-fits-all. It exists on a spectrum of intensity. Imagine a discomfort scale from 1 to 10: light opiate withdrawal symptoms might register as a 3 or 4. It’s a deeply uncomfortable and draining experience, but it’s often manageable without intensive medical intervention. In contrast, severe withdrawal can quickly escalate to an 8, 9, or 10, a range where the symptoms become debilitating, overwhelming, and potentially dangerous, making professional medical supervision essential.
The distinction between mild and severe withdrawal is not just about comfort—it’s fundamentally about safety. This process is triggered by physical dependence, a state where the body has adapted to the presence of opioids and requires them to function normally. It’s important to differentiate this from addiction. Physical dependence can happen to anyone taking opioids for a prolonged period, even as prescribed by a doctor. Addiction, on the other hand, is a complex brain disease characterized by compulsive drug-seeking and use despite harmful consequences.
To objectively measure where an individual falls on this spectrum, healthcare professionals use standardized tools like the Clinical Opiate Withdrawal Scale (COWS). This assessment evaluates 11 common signs and symptoms, including resting pulse rate, sweating, restlessness, pupil size, bone and joint aches, runny nose and tearing, GI upset, tremor, yawning, anxiety or irritability, and gooseflesh skin. By scoring each of these, clinicians can determine the severity of withdrawal and tailor the level of medical care accordingly.
| Feature | Mild Opioid Withdrawal Symptoms | Severe Opioid Withdrawal Symptoms |
|---|---|---|
| Symptoms | Uncomfortable but manageable physical symptoms: persistent muscle aches, restlessness, anxiety, runny nose, sweating, yawning, mild nausea, stomach cramps, diarrhea, goosebumps, fatigue, and noticeable drug cravings. Often compared to a bad case of the flu. | Debilitating and dangerous symptoms: intense and persistent vomiting and diarrhea leading to dehydration, severe muscle spasms and deep bone pain, profuse sweating, uncontrollable tremors, and in rare cases, seizures. This is coupled with extreme psychological distress, including panic attacks, paranoia, hallucinations, and overwhelming cravings. |
| Intensity | The discomfort is significant but does not typically incapacitate the individual. Daily functioning is difficult but may still be possible to a limited extent. The primary focus is on comfort and symptom management. | The intensity is overwhelming and incapacitating, making self-care impossible. The individual is often bedridden and unable to keep down food or fluids. The experience is physically and emotionally agonizing. |
| Risks | The primary risk is discomfort leading to a potential relapse to stop the symptoms. Dehydration is possible but can usually be managed with consistent fluid intake. Serious medical complications are rare. | High risk of life-threatening complications, including severe dehydration, dangerous electrolyte imbalances affecting heart function, aspiration (inhaling vomit) leading to pneumonia, and extreme psychological distress that can result in self-harm. The risk of overdose upon relapse is also critically high. |
Several factors determine whether you will experience mild or severe withdrawal. The duration of use is a primary factor; the brain and body of someone who has used opioids for months or years have undergone more significant neuroadaptation, leading to a more intense rebound effect. The type of opioid also plays a critical role. Short-acting opioids like heroin and fentanyl cause a rapid and intense withdrawal, while long-acting opioids like methadone lead to a more prolonged, drawn-out process. Finally, dosage is key; higher doses saturate more of the brain’s opioid receptors, resulting in a more severe withdrawal when the substance is removed.
Defining Light Opiate Withdrawal Symptoms
Light opiate withdrawal symptoms are most likely to occur when you’ve been using lower doses of opioids or for a shorter period. This milder experience is also the intended outcome when you work with a doctor to taper your medication gradually. Tapering allows your body to slowly adjust to lower levels of the opioid, softening the shock of its eventual absence.
The symptoms, while persistent and unpleasant, remain manageable for most. You may feel like you have a terrible flu—achy, tired, irritable, and generally unwell—but you can typically still get out of bed, drink fluids, and perform basic self-care. Crucially, there is an absence of severe complications like uncontrollable vomiting, dangerous levels of dehydration, or seizures. For many in Miami and across Florida, managing light withdrawal at home with a strong support system and professional guidance is possible, but it requires careful preparation and a solid plan.
The Dangers of Severe Withdrawal
Severe withdrawal is a medical crisis. The relentless vomiting and diarrhea make it impossible to stay hydrated, turning dehydration into a serious threat that can lead to kidney damage and other organ failure. This fluid loss also causes electrolyte imbalances, disrupting the delicate mineral balance that regulates nerve function and, most critically, your heart rhythm, potentially causing dangerous arrhythmias.
During episodes of intense nausea, aspiration—inhaling vomit into the lungs—can occur, leading to a dangerous infection called aspiration pneumonia. While seizures are much rarer in opioid withdrawal than in alcohol or benzodiazepine withdrawal, they can happen in extreme cases, particularly if there are co-occurring health issues.
The extreme psychological distress is one of the most challenging aspects. This isn’t just feeling anxious; it’s a state of profound terror, panic, and despair that can feel unbearable. This mental anguish, combined with overwhelming cravings, makes it nearly impossible to cope without professional intervention. Perhaps the most insidious danger is the increased overdose risk post-detox. An individual’s tolerance to opioids plummets during withdrawal. If they relapse in a moment of desperation, taking their previous dose can easily overwhelm their system, leading to a fatal overdose. In a place like Florida, with the widespread presence of potent fentanyl, this risk is tragically high.
This is precisely why professional medical supervision is not a luxury but a necessity when withdrawal symptoms escalate. At a dedicated facility like Summer House Detox Center, our experienced medical team can monitor your vital signs 24/7, manage symptoms with appropriate medications, and provide the safe, comfortable environment you need to get through the most difficult phase of recovery. Understanding where you fall on this spectrum can help you make the life-saving decision to seek the right level of care for your symptoms of opiate withdrawal.
