Understanding Benzodiazepine Withdrawal: Why Professional Management Matters

Benzo withdrawal management is the medically supervised process of safely discontinuing benzodiazepine medications to prevent dangerous symptoms. If you’ve taken benzos like Xanax, Ativan, or Valium daily for over a month, your body has likely developed physical dependence. Stopping suddenly can be life-threatening.
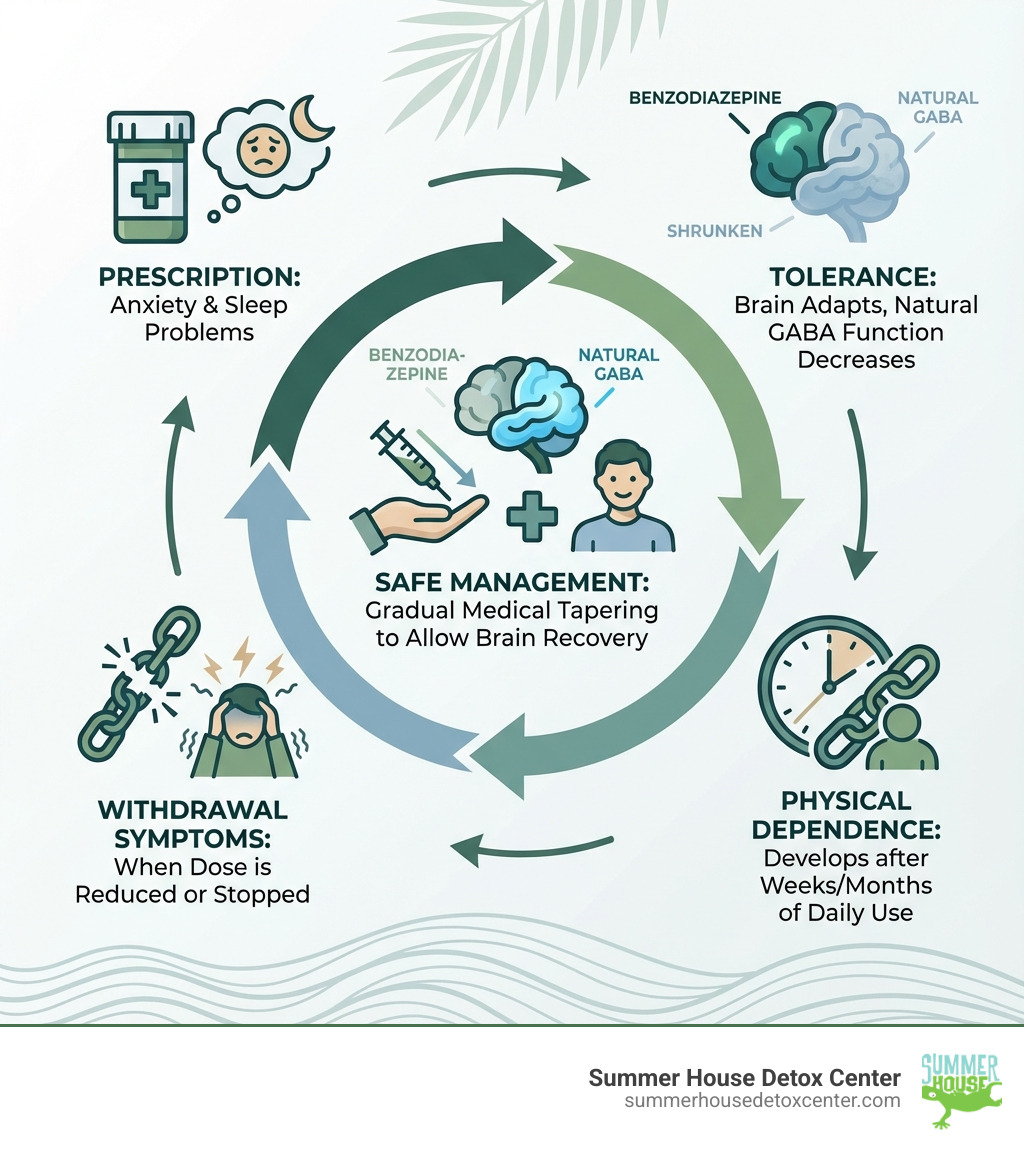
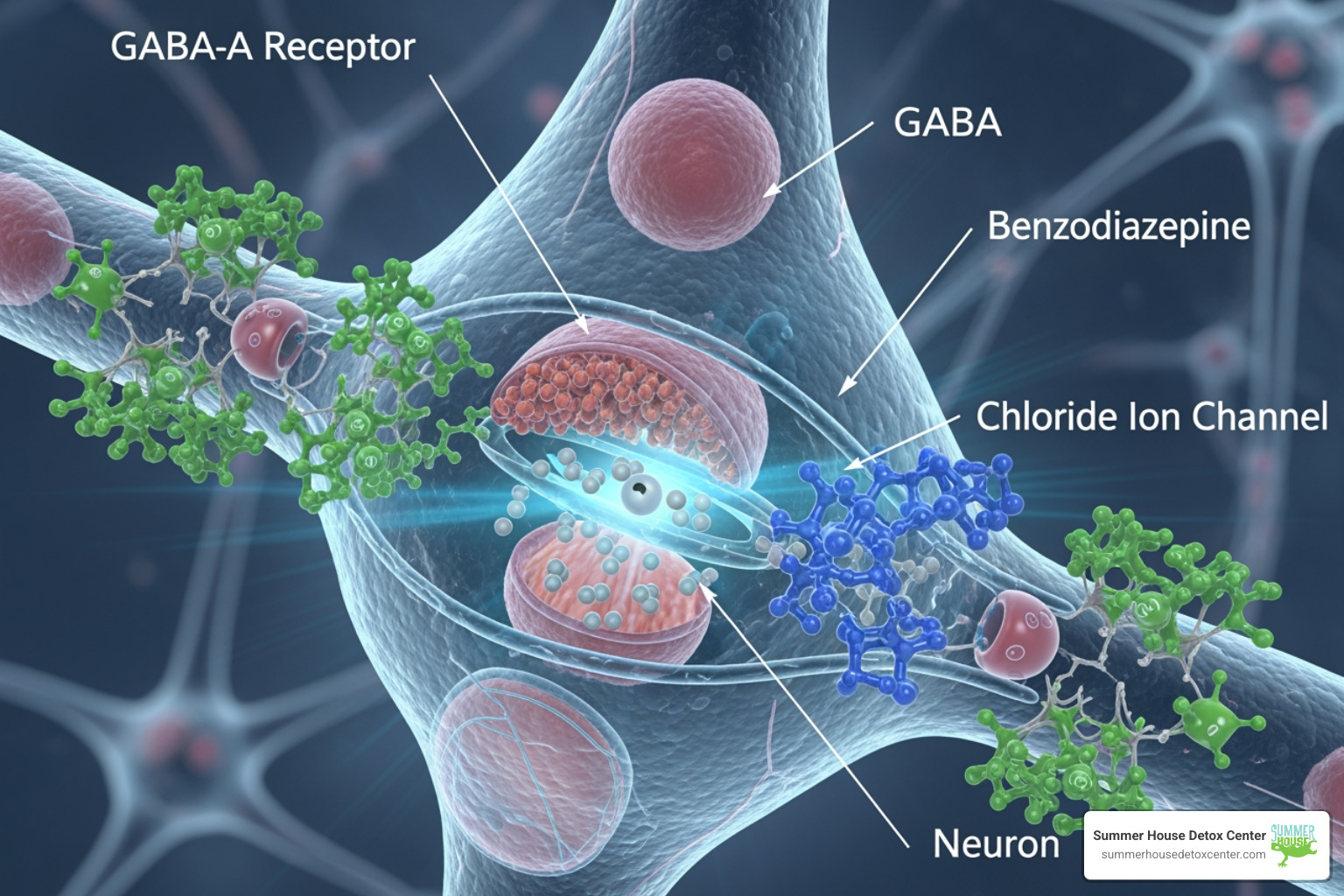
This physical dependence is a normal biological response, not a moral failing. These medications improve your brain’s calming system (GABA receptors), but with extended use, the brain adapts and relies on the drug. Over time, tolerance builds, the medication becomes less effective, and stopping causes severe withdrawal, trapping many users.
Key Components of Safe Benzo Withdrawal Management:
- Gradual tapering: Slowly reducing dosage over weeks or months.
- Medical supervision: Constant monitoring by healthcare professionals.
- Symptom management: Addressing anxiety, insomnia, and physical discomfort.
- Individualized schedules: Customizing the taper based on your response.
- Support systems: Combining medical care with counseling and peer support.
Abrupt discontinuation can trigger seizures, psychosis, and other life-threatening complications. In Florida’s warm climate, dehydration can worsen these symptoms. That’s why professional benzo withdrawal management in Miami, Fort Lauderdale, and across the state is essential, focusing on gradual tapering with expert support.
This guide covers withdrawal symptoms, timelines, treatment options, and resources to help you or a loved one safely break free from benzodiazepine dependence.
Understanding Benzodiazepine Withdrawal: Symptoms, Timeline, and Risks
Benzodiazepines boost the effects of GABA, our brain’s primary calming neurotransmitter. With prolonged use, the brain adapts to this chemical boost in a process called neuroadaptation. It becomes less efficient at producing its own calming effects and relies on the medication to maintain balance. When the drug is removed, the brain is left in a hyperexcitable state, causing withdrawal symptoms.
It’s important to distinguish between “rebound” symptoms (a temporary worsening of original issues like anxiety) and true withdrawal, which involves a new set of symptoms reflecting the brain’s struggle to rebalance. True withdrawal can be far more severe, making effective benzo withdrawal management critical. For more on the science, see the Treatment of Benzodiazepine Dependence.
What are the primary symptoms of benzodiazepine withdrawal?
Withdrawal symptoms can be varied and unsettling, affecting both mind and body. Understanding them is the first step in proper benzo withdrawal management.
Common psychological symptoms include:
- Intense anxiety and panic attacks
- Irritability and agitation
- Depression and suicidal ideation
- Confusion and memory problems
- Hypersensitivity to noise or light
- Feelings of detachment (depersonalization/derealization)
- In severe cases, psychosis or hallucinations
Common physical symptoms include:
- Insomnia and nightmares
- Muscle spasms, aches, and stiffness
- Hand tremors
- Excessive sweating
- Nausea, vomiting, and weight loss
- Headaches and tinnitus (ringing in the ears)
- Heart palpitations
- Burning or tingling skin sensations
The intensity of symptoms varies per person. For a comprehensive overview, see The benzodiazepine withdrawal syndrome.
Withdrawal Timeline and Influencing Factors
The withdrawal timeline depends heavily on the type of benzodiazepine used:
- Short-acting benzodiazepines (e.g., alprazolam, lorazepam): Withdrawal can start within 2-4 days and the acute phase may last 4-7 days. The onset is rapid and intense.
- Long-acting benzodiazepines (e.g., diazepam): Withdrawal onset is delayed to 4-7 days, with the acute phase lasting 7-14 days. The onset is slower, but the duration can be prolonged.
Severity and duration are also influenced by:
- Duration of use: Longer use often means a more challenging withdrawal.
- Dosage: Higher doses usually lead to more severe symptoms.
- Individual factors: Personal metabolism, overall health, and co-occurring mental health disorders play a significant role.
- Polysubstance use: Using other depressants like alcohol or opioids complicates withdrawal and increases risks.
Understanding these factors is key to tailoring an effective benzo withdrawal management plan. More details can be found in Pharmacokinetic Properties of Benzodiazepines.
Potential Complications and Dangers
Attempting to stop “cold turkey” without medical supervision is extremely dangerous. Immediate medical access in Florida can be critical to manage severe complications.

The most severe potential complications include:
- Seizures: Abrupt cessation can trigger generalized seizures, which can be fatal. This risk is highlighted in studies such as Death following suspected alprazolam withdrawal seizures.
- Psychosis and Hallucinations: Severe mental disturbances that require immediate professional intervention.
- Delirium: A state of acute confusion and altered consciousness that is a medical emergency.
- Catatonia: A complex syndrome affecting movement and behavior that requires specialized care.
- Suicidal Ideation: Intense depression and hopelessness can significantly increase suicide risk.
These risks are why professional benzo withdrawal management is essential for safety.
Physical Dependence vs. Benzodiazepine Use Disorder (BUD)
It’s vital to distinguish between physical dependence and a benzodiazepine use disorder (BUD), or addiction.
Physical dependence is a normal physiological adaptation. It means withdrawal symptoms will occur if the drug is stopped. This can happen even when taking the medication exactly as prescribed. It is not a sign of addiction.
A Benzodiazepine Use Disorder (BUD) is a more complex condition involving compulsive drug use despite harmful consequences. According to the DSM-5, it includes criteria like loss of control over use and continued use despite negative life impacts.
Fortunately, research suggests only a small percentage (around 1.5%) of individuals prescribed benzodiazepines develop a BUD, according to Prevalence and Correlates of Benzodiazepine Use. This distinction helps reduce stigma and encourages people to seek benzo withdrawal management without shame.
The Core of Benzo Withdrawal Management: Tapering Strategies
Successful benzo withdrawal management is a patient-centered, collaborative journey between you and your healthcare team. The goal is to get you off the medication safely and comfortably. The process is often slow and non-linear, and flexibility is key to preventing severe withdrawal and ensuring success.
This philosophy of shared decision-making is stressed in guidelines like The Joint Clinical Practice Guideline on Benzodiazepine Tapering.
The Gold Standard: Gradual Tapering
Gradual tapering is the safest and most effective method. It involves slowly reducing the benzodiazepine dose over an extended period, allowing your brain to readjust. The pace must be individualized.
While some might tolerate a 25% dose reduction every 2–4 weeks, others may need a much slower pace, like a 5% reduction every 4–6 weeks. The American Society of Addiction Medicine (ASAM) suggests initial reductions of 5-10% every 2-4 weeks. The “tail-end” of the taper, at very low doses, is often the most challenging phase. For some, the entire process may last more than a year, requiring patience and close medical collaboration. This approach is reinforced by resources like the New Benzodiazepine Tapering Guide – Slow and Patient Centered.
The Role of Long-Acting Benzodiazepines in Tapering
A common strategy in benzo withdrawal management is switching from a short-acting benzodiazepine to a long-acting one like diazepam (Valium). Short-acting benzos cause sharp drops in blood levels, leading to more intense withdrawal between doses. Long-acting benzos provide a smoother, more stable level of medication, creating a gentler withdrawal curve.
A medical team calculates an equivalent dose using a Benzodiazepine Dose Equivalents chart. Once you are stable on the new medication, the gradual taper begins. This method allows for more precise adjustments and minimizes shock to your system, as guided by tools like Tapering Flowcharts.
Managing Protracted Withdrawal Symptoms (PAWS)
While acute withdrawal lasts weeks, some individuals experience Protracted Withdrawal Syndrome (PAWS), where symptoms linger for months or even years. This reflects the profound neuroadaptation from long-term use.
Common protracted symptoms include:
- Persistent tinnitus, anxiety, and insomnia
- Cognitive deficits (e.g., memory problems)
- Gastrointestinal issues
- Tingling or burning sensations (paresthesia)
- Muscle pain and tremors
- Dizziness and depression
The duration of PAWS varies, and research notes there’s “no known cure” except time and support. Coping strategies focus on acceptance, symptom management, and resilience:
- Acceptance: Understanding symptoms are temporary reduces fear.
- Support Systems: Therapy, support groups, and loved ones are crucial.
- Lifestyle Adjustments: Healthy diet, exercise, and stress-reduction techniques help manage symptoms.
- Patience: The brain needs time to heal.
Effective benzo withdrawal management prepares individuals for PAWS with strategies and support for this challenging phase.
Professional Treatment: Inpatient Withdrawal Management in Florida
Choosing the right level of care for benzo withdrawal management is a critical decision. For many, a medically supervised inpatient program offers the safest path. At Summer House Detox Center in Miami, FL, we prioritize your safety and comfort in a serene environment designed for healing.
We begin with a thorough assessment to create a detox plan customized to your needs, medical history, and benzodiazepine use patterns, providing a peaceful setting for recovery in Florida.
When is Inpatient Detox Necessary?
While some can taper as an outpatient, certain factors increase the risk of severe complications, making inpatient detox the essential choice.
We recommend inpatient benzo withdrawal management for high-risk factors such as:
- High Dosage: Taking over 50mg diazepam equivalent per day.
- Polysubstance Use: Also using other depressants like opioids or alcohol.
- History of Seizures or Delirium: Previous severe withdrawal reactions.
- Severe Mental Illness: Co-occurring conditions like psychosis or bipolar disorder.
- Lack of Home Support: An unstable or unsupportive home environment.
- Rapid Discontinuation: Attempting to stop “cold turkey.”
The 24/7 medical care at a facility like Summer House Detox Center in Miami, FL, is invaluable. Our staff continuously monitors you, adjusting medication as needed to ensure your safety and comfort. For more on our services, you can visit our page: More info about inpatient detox services.
Recommended Inpatient Benzo Withdrawal Management
Our approach at Summer House Detox Center is a medically supervised detox rooted in best practices and personalized care.
Our inpatient management typically involves:
- Medically Supervised Detoxification: A thorough assessment upon admission creates your personalized detox plan.
- Stabilization: We often convert your current benzo to an equivalent dose of a long-acting one, like diazepam, to ease the taper.
- Gradual Tapering Schedule: We initiate a slow, carefully calculated taper, often a 10mg diazepam equivalent reduction per day, always adjusted based on your response.
- Symptom-Triggered Protocols: Our staff responds immediately to emerging symptoms, making prompt adjustments to manage discomfort.
- Adjunct Medications: We may use non-addictive medications to manage specific symptoms like nausea or insomnia under strict medical guidance.
- Continuous Monitoring: Our experienced team relies on frequent patient interaction, symptom assessment, and vital sign checks to guide your care in real-time.
Our team at Summer House Detox Center in Miami, FL, provides compassionate, evidence-based care for your benzo withdrawal management journey.
Outpatient Benzo Withdrawal Management: A Collaborative Approach
Outpatient benzo withdrawal management can be a suitable option for individuals with lower risk factors and strong support systems. This collaborative approach requires a committed partnership with your clinician.
Outpatient management is generally for patients who:
- Are on lower doses of benzodiazepines.
- Have no history of severe withdrawal complications.
- Have stable physical and mental health.
- Have a safe and supportive home environment.
Success relies on a strong doctor-patient relationship, an individualized tapering schedule, regular check-ins, and family involvement. While Summer House Detox Center is an inpatient facility, we understand the importance of a full continuum of care and can provide guidance on accessing appropriate outpatient resources in Florida as you transition from our program.
Special Considerations and Adjunctive Support
Effective benzo withdrawal management requires tailoring treatment to address unique vulnerabilities. Certain populations and adjunctive therapies are crucial for a holistic approach to recovery.
Tapering in Special Populations
Some groups require highly specialized approaches due to unique vulnerabilities.
- Older Adults: This group metabolizes medications more slowly, increasing risks of falls, cognitive impairment, and over-sedation. Tapering schedules must be significantly slower, with lower starting doses and gradual reductions. Many older adults experience improved health after successfully withdrawing, as noted in a SAMHSA Letter on Older Adults.
- Pregnant Women: Managing withdrawal during pregnancy is a delicate balance. Abrupt discontinuation poses risks to both mother and fetus, but continued use can lead to neonatal abstinence syndrome (NAS). A multidisciplinary team must carefully weigh the decision to taper. For guidance, consult Pregnancy Considerations.
These populations highlight the need for a highly individualized, medically supervised approach.
The Role of Non-Pharmacological Interventions
While tapering is the cornerstone of benzo withdrawal management, non-pharmacological interventions are vital for managing symptoms and building long-term well-being.
- Cognitive Behavioral Therapy (CBT): Highly effective for addressing anxiety and negative thought patterns.
- Psychoeducation: Understanding the withdrawal process is empowering and reduces fear.
- Mindfulness and Relaxation Techniques: Deep breathing, meditation, and yoga can alleviate anxiety and improve sleep.
- Peer Support Groups: Connecting with others provides invaluable emotional support and reduces isolation.
- Healthy Diet and Exercise: A nutritious diet and regular physical activity support brain health and improve mood.
These psychosocial interventions are integral to a comprehensive plan, fostering resilience and sustainable recovery, as highlighted in studies on Psychosocial interventions for benzodiazepine dependence.
Helpful Resources for Patients and Clinicians
Navigating benzo withdrawal management can be overwhelming, but many resources exist to support patients and clinicians.
For Patients and Families:
- Patient Pocket Guide: A quick-reference digital tool with clear information on tapering: Patient Pocket Guide.
- Patient Infographic: A visual summary of safe tapering guidelines: Patient Infographic.
- Patient Handouts on Specific Medications: These materials are designed to inform and empower people about potentially inappropriate medications.
For Clinicians:
- ASAM Benzodiazepine Tapering Guideline: Comprehensive clinical guidelines for safe tapering: ASAM Benzodiazepine Tapering Guideline.
- VA Clinician’s Guide: A guide for providers, focusing on high-risk populations: VA Clinician’s Guide.
- Webinar Series and Microlearning Modules: Educational series for clinicians to gain expertise in safe tapering.
Frequently Asked Questions about Benzo Withdrawal
We understand you have many questions about benzo withdrawal management. Here are answers to some of the most common ones.
How long does benzo withdrawal last?
The duration is highly variable. It depends on the benzo type, dose, length of use, and individual physiology.
- Acute Phase: This is when symptoms are most intense. For short-acting benzos, it typically lasts 4-7 days. For long-acting ones, it can last 7-14 days. This phase requires close medical supervision.
- Protracted Withdrawal Syndrome (PAWS): Some individuals experience lingering symptoms (anxiety, insomnia, cognitive issues) for months or even years. These symptoms tend to wax and wane. While challenging, PAWS is not life-threatening and requires patience and ongoing support.
There is no fixed timeline, but proper benzo withdrawal management can safely guide you through the process.
Can you stop taking benzodiazepines cold turkey?
No. We strongly advise against stopping benzodiazepines “cold turkey.” Abrupt discontinuation is dangerous and can lead to life-threatening complications, including:
- Seizures
- Psychosis and hallucinations
- Delirium
- Severe rebound anxiety and panic
- Suicidal ideation
A gradual, medically supervised taper is the only safe method for discontinuing these medications. Medical supervision is absolutely crucial for benzo withdrawal management.
What helps with benzo withdrawal anxiety?
Anxiety is a primary withdrawal symptom. The most important strategy to manage it is a gradual taper, which allows your brain to adjust slowly and prevents sudden surges of anxiety.
Beyond the taper, these non-pharmacological methods offer significant relief:
- Cognitive Behavioral Therapy (CBT): Helps you develop new coping skills for anxious thoughts.
- Mindfulness and Relaxation: Practices like deep breathing and meditation calm the nervous system.
- Regular Physical Activity: Gentle exercise can reduce anxiety and improve mood.
- Healthy Diet and Hydration: Proper nutrition supports overall well-being and mood stability.
- Peer Support: Connecting with others who understand provides encouragement and reduces isolation.
In some cases, a doctor may prescribe non-addictive adjunct medications to manage severe anxiety during withdrawal. Always discuss any new medications with your healthcare provider.
Conclusion
Navigating benzodiazepine withdrawal is challenging, but it is manageable with the right support. A gradual, patient-centered, and medically supervised tapering strategy is the gold standard for safe and effective benzo withdrawal management. You do not have to face this journey alone, and the risks of abrupt cessation are too severe to attempt it without professional help.
Whether you’re in Miami, Fort Lauderdale, or anywhere in Florida, seeking professional guidance ensures your safety and comfort. At Summer House Detox Center, we provide personalized, medically supervised detox programs focused on your dignity and long-term recovery. Our experienced staff offers compassionate support every step of the way. If you’re ready to start a safe path to freedom from benzodiazepine dependence, we are here to help.
Find safe benzodiazepine detox in Florida
