Understanding the Reality Behind Rapid Heroin Detox
Rapid heroin detox, also known as Ultra-Rapid Opioid Detoxification (UROD) or anesthesia-assisted detox, is a procedure that promises to speed up withdrawal by administering opioid antagonists while a patient is under general anesthesia or heavy sedation. Here’s what you need to know:
Quick Facts About Rapid Heroin Detox:
- What it is: A 4-hour procedure using naloxone or naltrexone under anesthesia to force rapid withdrawal
- The promise: Avoid painful withdrawal symptoms by “sleeping through” detox
- The reality: Studies show it’s no more effective than standard detox methods
- Safety concerns: Serious adverse events including death, pulmonary edema, cardiac issues, and diabetic ketoacidosis
- Cost: $5,000 to $15,000, often not covered by insurance
- Expert consensus: Major health organizations recommend against it
- Long-term success: High relapse rates (14 of 16 patients in one study)
If you’re struggling with heroin addiction in Florida, you’ve likely felt desperate enough to consider any option that promises relief from the agony of withdrawal. The fear of those symptoms can keep people trapped in addiction for years. That’s why rapid detox centers market themselves so aggressively, offering what sounds like a miracle: go to sleep, wake up detoxed, skip the pain entirely.
But here’s the truth that marketing materials won’t tell you: anesthesia-assisted rapid opioid detoxification has been deemed unsafe and ineffective by nearly every major medical organization, including the American Society of Addiction Medicine and the National Institute on Drug Abuse.
A 2012 investigation by the New York City Department of Health found that out of 75 patients who underwent rapid detox at one clinic, two died and five others experienced life-threatening complications requiring hospitalization. That’s a serious adverse event rate of 9.3%. Meanwhile, a randomized trial published in JAMA found that patients who underwent anesthesia-assisted detox experienced withdrawal symptoms just as severe as those who used safer methods, and they were no more likely to stay in treatment or remain abstinent.
This article examines the science behind rapid heroin detox, separating fact from marketing hype. We’ll explore why this procedure gained popularity despite the evidence against it, what the real risks are, and most importantly, what safer alternatives exist for people seeking help in Miami and throughout Florida.
What is Anesthesia-Assisted Detox (UROD)?

Rapid heroin detox, often referred to as Ultra-Rapid Opioid Detoxification (UROD) or anesthesia-assisted detox, emerged as a controversial method promising a swift escape from the clutches of heroin dependence. The concept itself is designed to appeal to the understandable desire for a quick and “painless” solution to the agonizing experience of opioid withdrawal.
The Allure of a “Painless” Detox
The fear of intense and debilitating withdrawal symptoms is a significant barrier for many individuals considering recovery from heroin addiction. We understand this fear; the body’s dependence on opioids means that when the drug is stopped, the nervous system reacts intensely, leading to excruciating physical and psychological discomfort. This dread of withdrawal often keeps people trapped in a cycle of use, searching for any way to avoid the inevitable pain.
This is where the marketing promise of anesthesia-assisted detox comes in: the idea that you can simply “sleep through” the worst of the withdrawal, waking up with the physical dependence behind you. For individuals and families in crisis, desperate for a fast solution, this promise can be incredibly appealing, offering a guide of hope in a dark time.
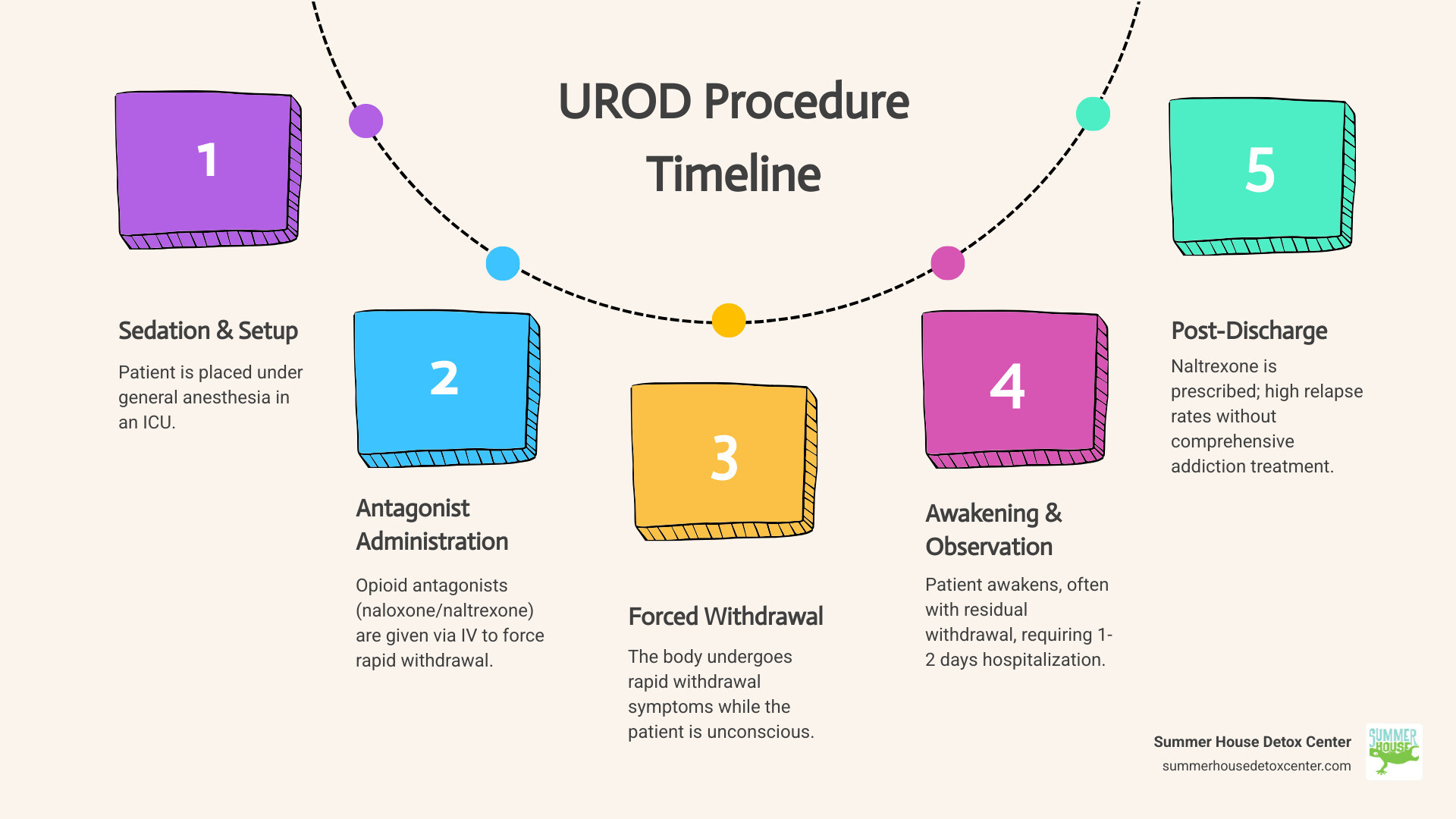
How the UROD Procedure Works
The core idea behind UROD is to accelerate the withdrawal process dramatically. Instead of a gradual tapering of opioids or a slow onset of withdrawal, UROD aims to compress the entire acute withdrawal phase into a matter of hours.
Here’s a general overview of how the UROD procedure typically works:
- General Anesthesia or Heavy Sedation: The patient is placed under general anesthesia or heavy sedation. This is intended to render them unconscious and unaware of the withdrawal symptoms that will be induced.
- Administration of Opioid Antagonists: While the patient is unconscious, high doses of opioid antagonists, such as naloxone or naltrexone, are administered intravenously. These medications rapidly block opioid receptors in the brain and body, effectively forcing any opioids that are present off these receptors.
- Induced Withdrawal: This rapid blockade of opioid receptors triggers an immediate and intense withdrawal syndrome. Because the patient is under anesthesia, they are purportedly shielded from the conscious experience of these symptoms.
- Compressed Timeline: The goal is to complete the most severe physical withdrawal in a few hours, typically ranging from 4 to 6 hours. Patients might then remain under medical supervision for a day or two in an intensive care unit (ICU) setting to monitor for complications.
- Post-Procedure Naltrexone: Following the procedure, patients are often discharged with oral naltrexone or an extended-release injectable form (like Vivitrol), which continues to block opioid receptors and is intended to prevent relapse by eliminating the euphoric effects of opioids.
The promise is that by rapidly flushing opioids from the system while the patient is unconscious, the physical hurdle of withdrawal can be overcome almost instantly. However, as we will explore, the reality often falls short of this optimistic picture, and the risks associated with this method are substantial. More information on these techniques can be found in reviews such as “Rapid and ultrarapid opioid detoxification techniques” from PubMed.
The Risks and Reality of Rapid Heroin Detox
Despite its appealing promise, anesthesia-assisted rapid heroin detox has faced intense scientific scrutiny and widespread condemnation from major health organizations. The scientific community largely views it as an unproven and high-risk procedure, with little to no evidence of superior effectiveness over safer, more established methods.
Significant Medical Dangers and Adverse Events
The very nature of anesthesia-assisted detox introduces a host of serious medical dangers. Administering high doses of opioid antagonists while a patient is under general anesthesia can provoke a severe physiological stress response.
Reported risks and adverse events associated with UROD, particularly when performed under anesthesia or heavy sedation, include:
- Risks of General Anesthesia: Any procedure requiring general anesthesia carries inherent risks, such as adverse reactions to medications, breathing problems, and cardiovascular complications.
- Respiratory Distress and Failure: Patients have experienced marked withdrawal symptoms, tachypnea (rapid breathing), and even respiratory distress during the acute post-anesthesia phase. This can escalate to pulmonary edema (fluid in the lungs) and aspiration pneumonia, especially if the patient vomits while sedated or recovering.
- Cardiovascular Complications: The sudden and intense withdrawal can lead to significant cardiovascular stimulation, including abnormal heart rhythms (cardiac arrhythmias) and profound increases in stress hormones like epinephrine, putting immense strain on the heart.
- Renal Failure: Cases of acute renal failure have been reported, alongside other metabolic disturbances like diabetic ketoacidosis, particularly in patients with underlying health conditions that may have been concealed.
- Neurological and Psychiatric Effects: Delirium, psychosis, and a bipolar mixed state have been observed following UROD. These severe psychological disturbances can increase the risk of self-harm or violent behavior.
- Electrolyte Imbalances: Severe vomiting and diarrhea, common during intense withdrawal, can lead to dangerous electrolyte disturbances, such as hypokalemia (low potassium), which can contribute to cardiac issues.
- Infections and Other Complications: In some cases, patients have developed severe infections like sepsis or necrotizing fasciitis, possibly linked to the overall stress on the body or complications during the procedure.
- Patient Deaths: Tragically, several deaths have been reported in association with anesthesia-assisted rapid detox procedures. An investigation highlighted two deaths and five hospitalizations among just 75 patients at one clinic, resulting in a 9.3% serious adverse event rate.
These serious adverse events underscore the significant and often life-threatening risks inherent in this approach. As detailed in “Guidelines for Rapid Detoxification from Opioids,” proper medical supervision and facility capacity for severe withdrawal are critical for any rapid detox method, but the combination with anesthesia adds layers of risk that are often deemed unacceptable.
What Does the Evidence Say About Rapid Heroin Detox?
When we look at the scientific evidence, the picture for anesthesia-assisted rapid heroin detox becomes even clearer: it does not offer superior outcomes.
A randomized controlled trial comparing anesthesia-assisted detox to buprenorphine-assisted and clonidine-assisted methods for heroin dependence found that while anesthesia-assisted detox achieved high rates of naltrexone induction, it was associated with significant withdrawal symptoms comparable to the alternative methods. Crucially, it did not lead to better treatment retention or abstinence rates. In fact, serious adverse events were concentrated in the anesthesia-assisted group, including pulmonary edema, aspiration pneumonia, diabetic ketoacidosis, and a bipolar mixed state. The study concluded that the data do not support the use of general anesthesia for heroin detoxification.
Furthermore, a structured evidence review by Gowing et al. (2010) concluded that “heavy sedation compared to light sedation does not confer additional benefits in terms of less severe withdrawal or increased rates of commencement on naltrexone maintenance treatment.” The review also noted that antagonist-induced withdrawal under heavy sedation or anesthesia is not supported due to potential life-threatening adverse events and high costs. An UpToDate review in 2013 echoed these concerns, stating that “serious complications have been reported with anesthesia-assisted rapid detoxification, and a randomized trial did not find it to be superior to buprenorphine-assisted rapid detoxification, or clonidine-assisted detoxification.” It further advised that ultrarapid opiate detoxification is not a medically sound therapy and should be avoided.
Even the Canadian Agency for Drugs and Technologies in Health (2016) found that “the evidence on clinical effectiveness and safety of UROD… were limited and of low quality.” This consistent lack of robust, positive evidence, coupled with significant safety concerns, leads to a unified stance from medical experts.
The Stance of Major Health Organizations
Given the substantial risks and lack of proven benefits, major health organizations and regulatory bodies have largely come out against the use of anesthesia-assisted rapid heroin detox.
- American Society of Addiction Medicine (ASAM): ASAM, a leading professional society for addiction specialists, has issued public policy statements that recommend against the use of anesthesia-assisted rapid opioid detoxification. Their position is that such procedures are not supported by scientific evidence for safety or effectiveness.
- California Technology Assessment Forum (CTAF): As early as 2002, the CTAF determined that rapid and ultra-rapid opiate detoxification does not meet their assessment criteria due to insufficient evidence of efficacy and significant safety concerns.
- National Institute for Health and Care Excellence (NICE): The UK’s NICE guidelines (2007) explicitly state that “ultra-rapid and rapid detoxification using precipitated withdrawal should not be routinely offered,” and specifically, UROD under general anesthesia or heavy sedation “must not be offered due to serious adverse event risks.”
- UpToDate: A widely respected, evidence-based clinical resource for healthcare professionals, UpToDate states that “ultrarapid opiate detoxification is not a medically sound therapy and should be avoided.”
The consensus among medical professionals and public health bodies is clear: anesthesia-assisted rapid heroin detox is an unproven and high-risk procedure that should generally be avoided. The perceived benefits are outweighed by documented dangers and a lack of evidence that it improves long-term recovery outcomes.
Long-Term Outcomes and Cost: A Reality Check
Beyond the immediate risks, it’s crucial to examine the long-term effectiveness and financial implications of rapid heroin detox. The unfortunate truth is that even if a patient survives the procedure without immediate complications, the journey to lasting recovery is far from over, and the costs can be staggering.
Long-Term Abstinence and Relapse Rates
One of the most significant misconceptions surrounding rapid heroin detox is that it’s a “cure” for addiction. We know that detoxification, while a vital first step, is not recovery. Heroin addiction is a complex chronic disease that involves profound changes in brain chemistry and behavior. Simply removing the physical dependence does not address the underlying psychological and behavioral components of addiction.
Studies have consistently shown alarmingly high relapse rates following anesthesia-assisted detox. For example, one study reported that after a period of at least 30 months, only two out of 16 patients never relapsed and reported total opiate abstinence. A staggering 14 patients relapsed, with 12 of them eventually being prescribed methadone substitution programs and two continuing to use heroin. Another randomized trial noted an overall dropout rate of 82% across all rapid detox methods, with no significant difference in treatment retention between anesthesia-assisted detox (20%) and buprenorphine-assisted detox (24%) at 12 weeks.
These statistics highlight a critical flaw: while the physical withdrawal might be compressed, the cravings and psychological dependence remain unaddressed. Without comprehensive post-detoxification treatment, including therapy and support, individuals lack the coping skills and behavioral changes necessary to maintain long-term sobriety. This makes the allure of a quick fix a dangerous illusion.
The Prohibitive Cost of Rapid Heroin Detox
The financial burden of anesthesia-assisted rapid heroin detox is another significant deterrent, especially considering its questionable efficacy and substantial risks. The anesthesia method is prohibitively expensive, with most centers charging between $5,000 and $15,000 for the procedure. Some facilities have even been reported to charge upwards of $21,000.
What makes this cost even more concerning is that these procedures are often not covered by insurance. Many insurance providers, including major ones like Aetna, classify UROD as “experimental, investigational, or unproven” due to the lack of established effectiveness and safety concerns. This means individuals and families often pay out-of-pocket for a treatment that is not only risky but also largely ineffective in achieving lasting recovery.
When we consider the potential for serious complications requiring additional hospitalization, critical care, and ongoing medical management, the true costs can skyrocket even further. This financial strain, combined with the high likelihood of relapse, makes anesthesia-assisted detox an economically unsound choice for most.
Here’s a simplified comparison:
| Feature | Anesthesia-Assisted Rapid Detox (UROD) | Medically-Supervised Detox (e.g., at Summer House Detox Center) |
|---|---|---|
| Primary Goal | Rapidly force withdrawal while unconscious | Safely manage withdrawal symptoms to achieve physical stability |
| Method | General anesthesia + opioid antagonists | Medications (buprenorphine, clonidine, comfort meds) + 24/7 medical care |
| Duration of Acute W/D | Hours (while unconscious) | Days to a few weeks (depending on substance and individual) |
| Conscious W/D Pain | Supposedly none (but often present post-anesthesia) | Managed with medication for comfort and safety |
| Key Risks | Death, respiratory/cardiac failure, psychosis, aspiration, DKA | Minimal risks when medically supervised; discomfort |
| Effectiveness | No more effective than other methods for long-term recovery | High success rate for initial detoxification and transition to treatment |
| Long-Term Relapse Rate | Very High (without follow-up care) | Significantly lower with integrated follow-up treatment |
| Cost | Very High (often out-of-pocket) | Often covered by insurance; more cost-effective overall |
| Medical Consensus | Not recommended, unproven | Gold standard of care for opioid withdrawal |
Safer, Evidence-Based Alternatives for Heroin Detox
Fortunately, for individuals in Florida seeking help for heroin addiction, there are safe, effective, and evidence-based alternatives to rapid heroin detox that prioritize patient well-being and long-term recovery. At Summer House Detox Center in Miami, we believe in a humane approach that sets the foundation for lasting sobriety.
Medically-Supervised Detoxification
The gold standard for opioid withdrawal is medically-supervised detoxification. This approach involves 24/7 medical monitoring in a safe, inpatient setting. Our experienced medical team, many of whom are in recovery themselves, understands the challenges of withdrawal and is dedicated to making the process as comfortable and dignified as possible.
During medically-supervised detox, we focus on:
- Symptom Management: We use proven medications to alleviate the often severe and uncomfortable symptoms of heroin withdrawal symptoms, such as nausea, vomiting, muscle aches, and anxiety. This helps prevent complications and reduces suffering.
- Patient Comfort and Stability: Our priority is the patient’s well-being. We provide a supportive environment where individuals can safely steer withdrawal without the added risks of anesthesia or heavy sedation.
- Personalized Care: Every individual’s journey is unique. We tailor our detox plans to meet specific needs, considering the type and amount of opioid used, duration of dependence, and any co-occurring physical or mental health conditions.
- Transition to Treatment: Detox is the critical first step, but it’s just the beginning. We prepare patients for the next phase of their recovery, which involves comprehensive addiction treatment.
This approach, unlike anesthesia-assisted detox, does not rush the body’s natural healing process but supports it, ensuring that patients are medically stable and ready to engage in further treatment. This is the foundation of our medically supervised withdrawal programs at Summer House Detox Center.
The Critical Role of Post-Detox Treatment
We cannot emphasize this enough: detoxification is not recovery. It is merely the process of safely removing substances from the body and managing withdrawal. The true work of recovery begins after detox. Without comprehensive post-detoxification treatment and psychosocial support, the likelihood of relapse remains extremely high, regardless of how “rapid” the detox was.
At Summer House Detox Center, we integrate post-detox planning into every patient’s journey. This includes:
- Psychosocial Support: Addiction is often intertwined with psychological, emotional, and social factors. Therapy helps individuals explore the root causes of their addiction, develop healthier coping mechanisms, and address co-occurring mental health disorders.
- Individual Therapy: One-on-one sessions with a therapist provide a confidential space to process emotions, identify triggers, and develop personalized strategies for relapse prevention.
- Group Counseling: Sharing experiences with peers who understand the struggle of addiction can be incredibly powerful. Group therapy fosters a sense of community, reduces isolation, and provides diverse perspectives on recovery.
- Relapse Prevention Planning: We equip our patients with practical tools and strategies to recognize warning signs, steer high-risk situations, and build a strong support network.
- Building a Foundation for Lasting Recovery: Our goal is to help individuals build a new life free from the grip of addiction, focusing on holistic well-being and sustained sobriety.
The treatment received after detoxification is consistently identified as the most important factor for long-term abstinence.
Proven Medications for Opioid Use Disorder
In addition to supportive care and psychosocial interventions, several medications have been rigorously studied and proven effective in treating opioid use disorder, both during and after detoxification. These medications are a cornerstone of evidence-based treatment and are vastly safer and more effective than anesthesia-assisted detox.
- Buprenorphine: This medication is a partial opioid agonist, meaning it activates opioid receptors but to a lesser degree than full agonists like heroin. It helps to reduce withdrawal symptoms and cravings without producing the same euphoric effects, making it an excellent tool for heroin detox. A randomized trial found buprenorphine-assisted detoxification to be a safer and more effective alternative to anesthesia-assisted methods.
- Methadone: A full opioid agonist, methadone is used in maintenance treatment to reduce cravings and withdrawal symptoms and block the effects of other opioids. It is typically administered in highly regulated clinics.
- Clonidine: This non-opioid medication helps to alleviate many of the physical symptoms of opioid withdrawal, such as sweating, chills, muscle aches, and anxiety, by acting on the nervous system. While less effective for long-term abstinence than buprenorphine or methadone, it can be a valuable aid during the acute detox phase.
- Naltrexone: As an opioid antagonist, naltrexone blocks opioid receptors, preventing opioids from producing their effects. It can be administered orally or as an extended-release injection (Vivitrol) after detoxification is complete. Naltrexone is crucial for preventing relapse but must only be started once all opioids are out of the system to avoid precipitating severe withdrawal.
These medications, when used as part of a comprehensive treatment plan, offer a safe and effective pathway to recovery, far superior to the dangerous gamble of anesthesia-assisted detox.
Conclusion: Choosing a Safe Path to Recovery in Florida
The promise of a quick, painless fix for heroin addiction is deeply appealing, but as we’ve explored, rapid heroin detox under anesthesia (UROD) is a dangerous myth. It is an expensive, high-risk procedure that lacks scientific evidence of superior effectiveness and is actively discouraged by major medical organizations. The risks of death and severe adverse events are simply too high, and the long-term outcomes are often disappointing, with high rates of relapse due to the absence of comprehensive addiction treatment.
For those in Florida seeking a safe, medically supervised path to recovery, it’s crucial to choose a facility that prioritizes evidence-based care. At Summer House Detox Center in Miami, we offer personalized, medically supervised detox with a focus on comfort, dignity, and support. We understand the unique challenges of addiction and provide a compassionate environment where individuals can safely begin their journey to sobriety.
We emphasize a holistic approach that extends beyond the initial detox, preparing our patients for long-term success through continued therapy and support. If you or a loved one is struggling with heroin addiction in Florida, please reach out. There is a safe and effective path to recovery, and we are here to guide you every step of the way.
Learn more about our medically-supervised heroin detox program.

