Understanding the Reality of Alcohol Withdrawal
Alcohol detox symptoms arise when a person who drinks heavily suddenly stops or cuts back. As the brain and body readjust without alcohol, symptoms can range from mild anxiety to life-threatening complications like seizures. Understanding these symptoms is crucial for anyone in Miami or throughout Florida who is considering stopping alcohol use or supporting someone through this process.
The body’s response to alcohol withdrawal is complex and varies significantly from person to person. When alcohol consumption stops abruptly, the central nervous system, which has adapted to the constant presence of alcohol, suddenly finds itself in a state of hyperexcitability. This dramatic shift is what produces the wide range of withdrawal symptoms that can affect nearly every system in the body.
Common alcohol withdrawal symptoms include:
- Mild (6-24 hours): Anxiety, insomnia, nausea, headaches, hand tremors, sweating, loss of appetite, mild confusion
- Moderate (12-48 hours): Increased blood pressure, rapid breathing, confusion, irritability, hallucinations, mood swings, difficulty concentrating
- Severe (48-72 hours): Seizures, delirium tremens (DTs), extreme agitation, high fever, profound confusion, cardiovascular complications
If you’re in Miami or anywhere in Florida and experience severe symptoms like seizures or extreme confusion, seek immediate medical attention. Florida’s warm climate can exacerbate certain withdrawal symptoms, particularly dehydration and electrolyte imbalances, making professional medical supervision even more critical.
About 50% of people with alcohol use disorder experience withdrawal when they stop drinking. The severity depends on multiple factors including drinking duration, daily consumption amount, overall health status, and previous withdrawal experiences. Repeated unsupervised withdrawals can worsen symptoms over time through a phenomenon known as the “kindling effect,” where each withdrawal episode potentially becomes more severe than the last. This neurological adaptation is why medical supervision is essential for safety, particularly for those who have attempted to quit drinking multiple times in the past.
The physical manifestations of withdrawal are often accompanied by psychological symptoms that can be equally challenging. Many individuals experience intense cravings, depression, anxiety, and mood instability during this period. These psychological symptoms can persist longer than physical symptoms and often require ongoing support and treatment to manage effectively.
Know your alcohol detox symptoms terms:
Why Alcohol Withdrawal Happens: The Science Behind the Symptoms
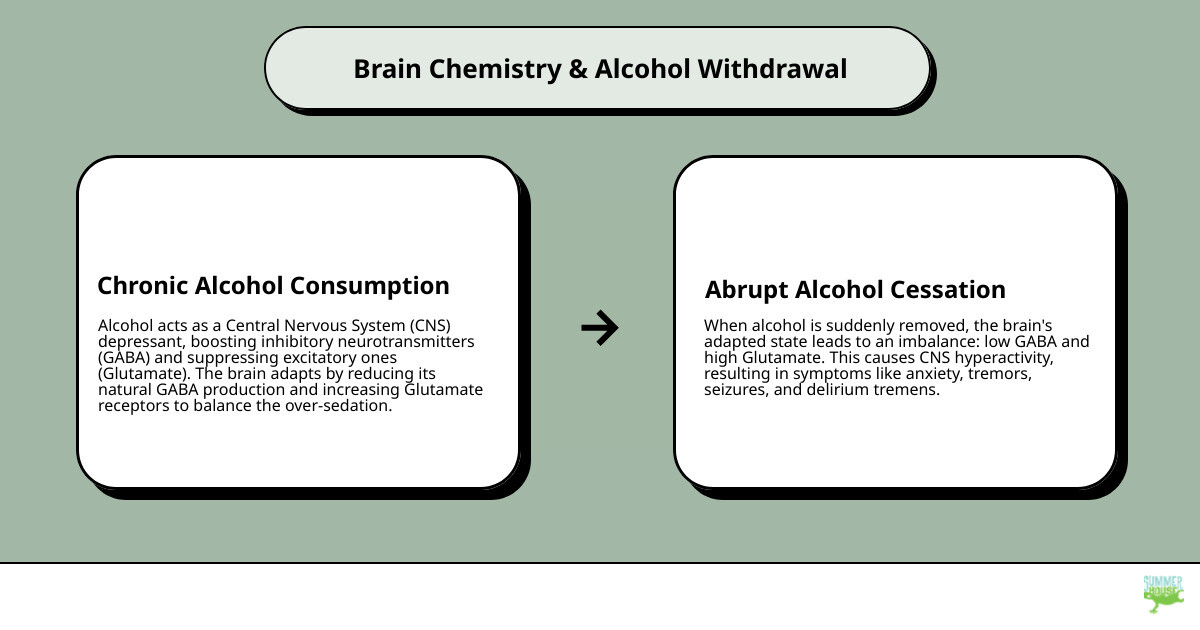
Alcohol is a central nervous system (CNS) depressant. Think of your brain having a brake pedal (GABA for calm) and a gas pedal (glutamate for alertness). Alcohol strengthens the brakes and eases off the gas. Over time, the brain adapts by weakening its own brakes and pressing the gas harder. When you suddenly stop drinking, youre left with weak brakes and a strong gas pedal, creating brain hyperactivity and the cascade of alcohol detox symptoms.
This also explains tolerance (needing more alcohol for the same effect). Understanding How Your Body Reacts to Alcohol Withdrawal helps. Research confirms that alcohol acts as a depressant on the central nervous system (CNS). Your symptoms are a physiological response, not a personal failingand with medical care, your brain can rebalance.
The Timeline of Alcohol Detox Symptoms

Knowing the typical time course can help you prepare mentally and physically for what lies ahead. While everyone’s experience is unique, this general pattern is common among those going through alcohol withdrawal. In Miami and throughout South Florida, medical professionals guide people through each step so they know what to expect as their body adjusts to functioning without alcohol.
The withdrawal timeline is not just a medical curiosity – it’s a roadmap that helps both patients and caregivers anticipate needs, prepare resources, and recognize when symptoms may require immediate intervention. Understanding this timeline can reduce anxiety about the unknown and help individuals make informed decisions about their care.
Stage 1: The First 6-12 Hours
Early warning signs typically begin within hours of the last drink and may include:
- Anxiety, restlessness, and insomnia
- Shaky hands (“the shakes”), sweating, and clammy skin
- Headaches, nausea, heart palpitations
- Mild disorientation and difficulty focusing
- Increased sensitivity to light and sound
- Initial cravings that may feel overwhelming
During this initial phase, many people in Florida’s recovery community report feeling a sense of impending doom or extreme nervousness. The body is beginning to recognize the absence of alcohol, and the nervous system starts to react. It’s crucial to stay hydrated during this phase, especially in Florida’s humid climate where sweating can quickly lead to dehydration.
Plan ahead for comfort and safety: The First 72 Hours of Detox: What to Expect and How to Prepare.
Stage 2: 12-48 Hours – Understanding Common Alcohol Detox Symptoms
Symptoms typically intensify during this critical period:
- Increased blood pressure and body temperature
- Rapid breathing, confusion, irritability
- Hallucinations (auditory, visual, tactile) that can be frightening
- Severe mood swings and emotional volatility
- Intense sweating and tremors
- Difficulty sleeping despite exhaustion
- Gastrointestinal distress including vomiting and diarrhea
This is often when people in South Florida realize professional help is needed. The symptoms during this phase can become overwhelming quickly, and the risk of complications increases significantly. Many individuals report that this period feels like the longest part of withdrawal, even though it typically lasts only 36 hours. The combination of physical discomfort and psychological distress can make it extremely difficult to cope without medical support.
Stage 3: 48-72 Hours – Peak Withdrawal
The highest-risk window may include:
- Seizures that can occur without warning
- Delirium Tremens (DTs) affecting 3-5% of those in withdrawal
- Marked agitation and disorientation
- Severe autonomic instability
- Potential for life-threatening complications
After 72 hours, symptoms typically begin to improve, though the journey is far from over. Some individuals may experience protracted withdrawal symptoms that can last weeks or even months. These post-acute withdrawal symptoms (PAWS) can include ongoing anxiety, sleep disturbances, and mood changes that require continued support and treatment.
Learn more about the complete timeline: Alcohol Detox: How Long Does It Take?.
Severe Symptoms: When to Seek Immediate Medical Help in Florida

Some alcohol detox symptoms are medical emergencies. Florida has excellent facilities for urgent caredont wait if youre concerned.
Delirium Tremens (DTs): A Medical Emergency
DTs typically appear 48 to 72 hours after the last drink. Signs include:
- High fever, rapid heart rate
- Severe confusion, disorientation, agitation
- Frightening hallucinations
- Seizures
Prompt treatment saves lives. See: Delirium Tremens (DTs) usually start 48-72 hours after stopping drinking. If DTs are suspected in Miami or anywhere in Florida, call 911 immediately.
Understanding Seizures and Other Severe Alcohol Detox Symptoms
Withdrawal seizures often occur within 24 to 48 hours. Repeated unsupervised withdrawals can worsen future episodes (the “kindling effect”). Severe dehydration and electrolyte imbalances can also trigger heart problems, especially in Floridas heat. Learn why professional care is safer: Why Choose Alcohol Detox at Rehab vs. at Home Detox.
How Alcohol Withdrawal is Diagnosed and Treated
In Florida – including here in Miami – comprehensive care starts with a thorough, nonjudgmental assessment. Medical professionals evaluate your drinking history (amount, frequency, last drink), prior withdrawal experiences, existing medical conditions, current medications, and support system. This detailed evaluation helps predict risk levels and allows for customized treatment planning that addresses your specific needs and circumstances.
The diagnostic process involves multiple components designed to ensure safe and effective treatment. Healthcare providers will typically conduct blood tests to check liver function, electrolyte levels, and overall health status. They may also perform an electrocardiogram (ECG) to assess heart function, as alcohol withdrawal can affect cardiovascular health. Mental health screening is equally important, as co-occurring disorders like anxiety or depression can complicate withdrawal and recovery.
Clinicians commonly use the Clinical Institute Withdrawal Assessment for Alcohol, Revised (CIWA-Ar) scale to guide care. This validated tool assesses ten areas including nausea, tremor, sweating, anxiety, agitation, tactile disturbances, auditory disturbances, visual disturbances, headache, and orientation. Typical cutoffs include: 8 or less (mild withdrawal), 8-15 (moderate withdrawal), and above 15 (severe withdrawal requiring intensive monitoring). If a person cannot participate due to confusion or other factors, alternative assessment tools like MINDS ensure proper evaluation. This systematic approach is why The Importance of Medically Supervised Detox: Why DIY Detox Can Be Dangerous cannot be overstated.
Medical Treatments and Medications
The primary goals of medical treatment are to keep you safe, prevent seizures and DTs, manage symptoms effectively, and make you as comfortable as possible throughout the withdrawal process. Treatment protocols are evidence-based and continuously adjusted based on your response.
- Benzodiazepines (such as Valium/diazepam, Ativan/lorazepam, Librium/chlordiazepoxide) are first-line medications to calm the overactive nervous system and prevent seizures. These medications work by enhancing GABA activity in the brain, essentially replacing alcohol’s calming effects temporarily while the brain rebalances.
- Phenobarbital may be used for severe cases or if benzodiazepines aren’t appropriate due to liver disease or other contraindications.
- Anti-seizure support such as Gabapentin can reduce anxiety and sleep issues while lowering seizure risk. Some facilities in Florida are increasingly using gabapentin as an adjunct therapy.
- Nutritional support is vital: thiamine (vitamin B1) replacement prevents Wernicke-Korsakoff syndrome, while correction of electrolytes (magnesium, potassium, sodium) protects the brain and heart. Many chronic drinkers are malnourished, making nutritional support essential.
- Symptom-specific medications may include anti-nausea drugs, blood pressure medications, and sleep aids as needed.
Care is adjusted in real time as symptoms change, with regular monitoring of vital signs and withdrawal severity. More on comfort-focused care: Managing Withdrawal Symptoms: How Summer House Detox Center Helps You Through the Hardest Days.
Supportive Care and Long-Term Recovery
The treatment setting and environment matter tremendously for successful recovery. In Miami’s recovery community, we prioritize:
- Continuous hydration and electrolyte monitoring, especially important in Florida’s climate
- Nutritional support with regular, balanced meals to restore physical health
- A calm, private environment that promotes rest and reduces sensory stimulation
- 24/7 monitoring by experienced medical staff familiar with withdrawal complications
- Counseling and emotional support starting during detox to address underlying issues
- Peer support from others in recovery who understand the journey
- Aftercare planning from day one, with connections to Florida resources like Alcoholics Anonymous and local support groups
- Family education and involvement when appropriate
- Coordination with outpatient providers for seamless transition to ongoing care
Detox is the crucial first step, but it’s just the beginning of the recovery journey. A personalized aftercare plan helps you transition to ongoing recovery and build a healthier, alcohol-free life in South Florida’s supportive recovery community.
ARTICLE SPECIFICATIONS
- Topic: alcohol detox symptoms
- Format: Extensive Guide
How Alcohol Withdrawal is Diagnosed and Treated
When you seek help for alcohol detox symptoms, clinicians in Miami and across Florida start with a focused assessment (history, exam, and risk review) and use tools like CIWA-Ar to guide care. This is why The Importance of Medically Supervised Detox: Why DIY Detox Can Be Dangerous matters.
Medical Treatments and Medications
- Benzodiazepines (for example, Valium and Ativan) are standard of care for safety and comfort.
- When needed, Phenobarbital or Gabapentin may be added.
- Thiamine and electrolyte replacement are routine to prevent complications.
More on our approach: Managing Withdrawal Symptoms: How Summer House Detox Center Helps You Through the Hardest Days.
Supportive Care and Long-Term Recovery
- Calm, safe setting
- Hydration, nutrition, and sleep support
- Counseling during detox and aftercare connections (including Alcoholics Anonymous)
Detox is only the beginning; we help you plan for sustained recovery.
RELEVANT STATISTICS
- Approximately half of those who suddenly stop or decrease their alcohol intake will experience alcohol withdrawal.
- Approximately one in 10 people with alcohol withdrawal syndrome are affected by seizures.
- If left untreated, up to one in three of these patients go on to experience delirium tremens.
- While only approximately 3% to 5% of patients with alcohol withdrawal syndrome will progress to alcohol withdrawal delirium, this condition may prove fatal.
- A 2013 sample of over 450,000 veterans’ hospital admissions found that 1 in 17 admitted patients were treated for alcohol withdrawal syndrome.
- Historically, the mortality rate of alcohol withdrawal delirium has been as high as 20%, but with advances in critical care, prompt diagnosis, and treatment, the rate is now around 1%.
KEY SOURCES AND SEO INSIGHTS
Key sources informing this guide:
- HSE (Health Service Executive Ireland): Alcohol withdrawal symptoms
- WebMD: Alcohol Withdrawal Symptoms, Timeline, and Treatment
- MyHealth.Alberta.ca: Alcohol Detoxification and Withdrawal: Care Instructions
- Drinkaware (UK): Alcohol withdrawal
- StatPearls (NIH/NLM): Alcohol Withdrawal Syndrome
- Cleveland Clinic: Alcohol Withdrawal
These clinical references align with our Miami- and Florida-based care model and reinforce best practices for safe, medically supervised detox.
