Understanding How Medication Can Support Your Recovery
Addiction medication therapy is a treatment approach that combines FDA-approved medications with counseling and behavioral therapies to treat substance use disorders. If you’re struggling with addiction and wondering whether medication could help you recover, here’s what you need to know:
Quick Answer: What is Addiction Medication Therapy?
- What it is: A “whole-patient” approach using medication plus therapy to treat addiction as a chronic disease
- How it works: Medications reduce cravings, ease withdrawal symptoms, and block the euphoric effects of substances
- What it treats: Opioid use disorder, alcohol use disorder, and nicotine addiction
- Key medications: Methadone, buprenorphine (Suboxone), naltrexone (Vivitrol), acamprosate, disulfiram
- The results: Improved survival rates, better treatment retention, reduced substance use, and increased ability to work and maintain relationships
Feeling overwhelmed by past failed attempts or withdrawal fears is common. Millions of Americans struggle with substance use disorders, and research shows combining medication with counseling dramatically improves recovery outcomes.
Here in Florida, including Miami, treatment centers offer these evidence-based programs supervised by experienced medical professionals. These medications aren’t “trading one drug for another”—they’re FDA-approved treatments that help normalize your brain chemistry so you can focus on healing.
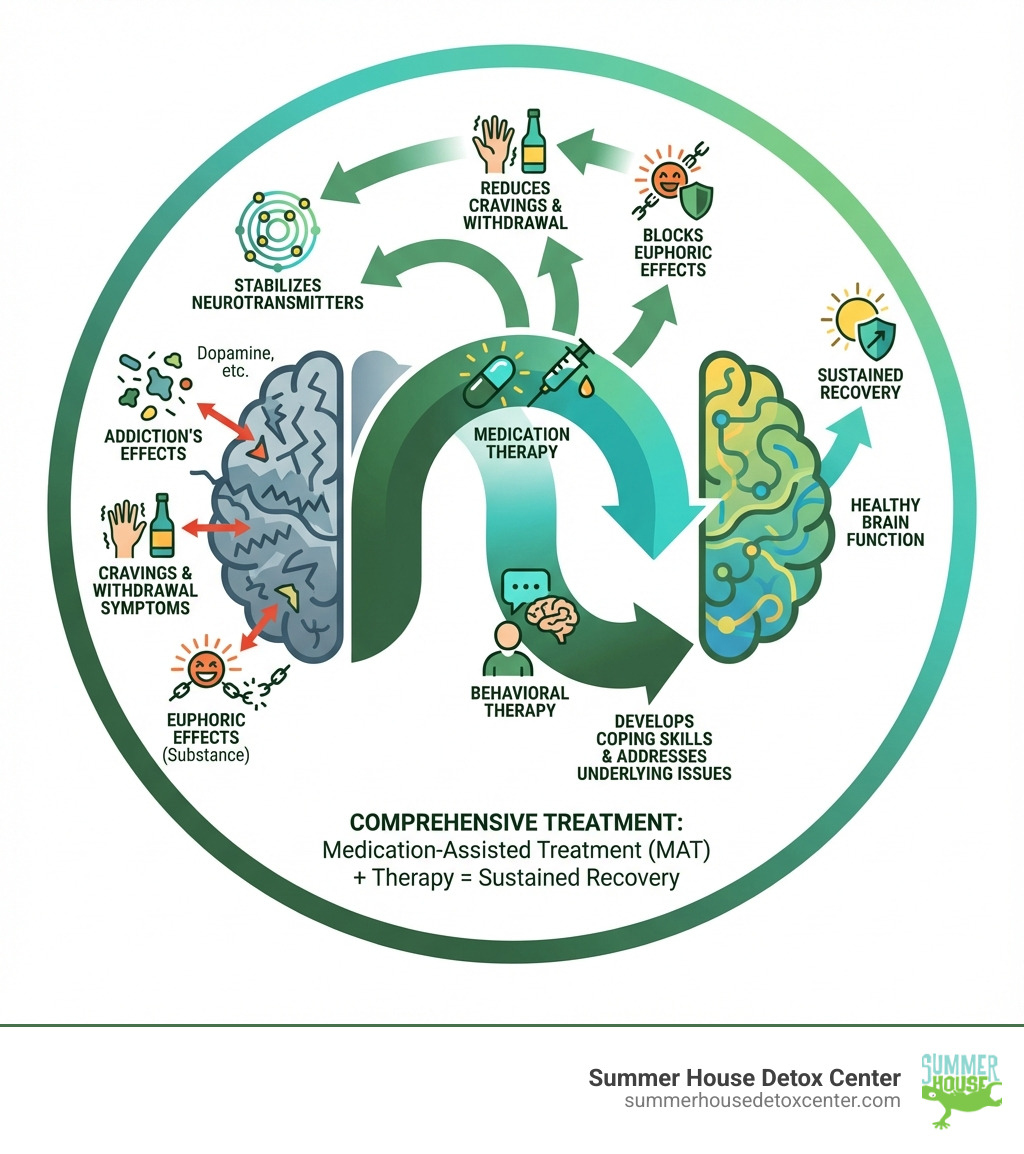
The chronic disease model of addiction recognizes that substances change your brain’s reward, motivation, and memory circuits. Medication-assisted treatment (MAT) addresses these biological changes while behavioral therapies help you develop coping skills for underlying issues.
Recovery is possible. With the right combination of medication, counseling, and support, you can regain control of your life.
What is Medication-Assisted Treatment (MAT)? A Foundation for Recovery
Addiction medication therapy is often called Medication-Assisted Treatment (MAT). It’s a comprehensive, “whole-patient” approach combining FDA-approved medications with counseling and behavioral therapies. MAT treats addiction as a chronic disease, addressing both the physical and psychological aspects of a substance use disorder (SUD).
Addiction is a complex brain disease, not a moral failing. Long-term substance use changes the brain’s structure and function, affecting reward, motivation, and self-control. This makes it incredibly difficult to simply stop using, even when facing severe consequences.
The primary goals of MAT are clear:
- Reducing cravings: Medications can significantly lessen the intense urges that often lead to relapse.
- Preventing withdrawal: They help manage the uncomfortable and sometimes dangerous symptoms of withdrawal, making detox safer and more tolerable.
- Normalizing brain chemistry: By acting on specific brain receptors, these medications help restore balance to brain functions disrupted by prolonged substance use.
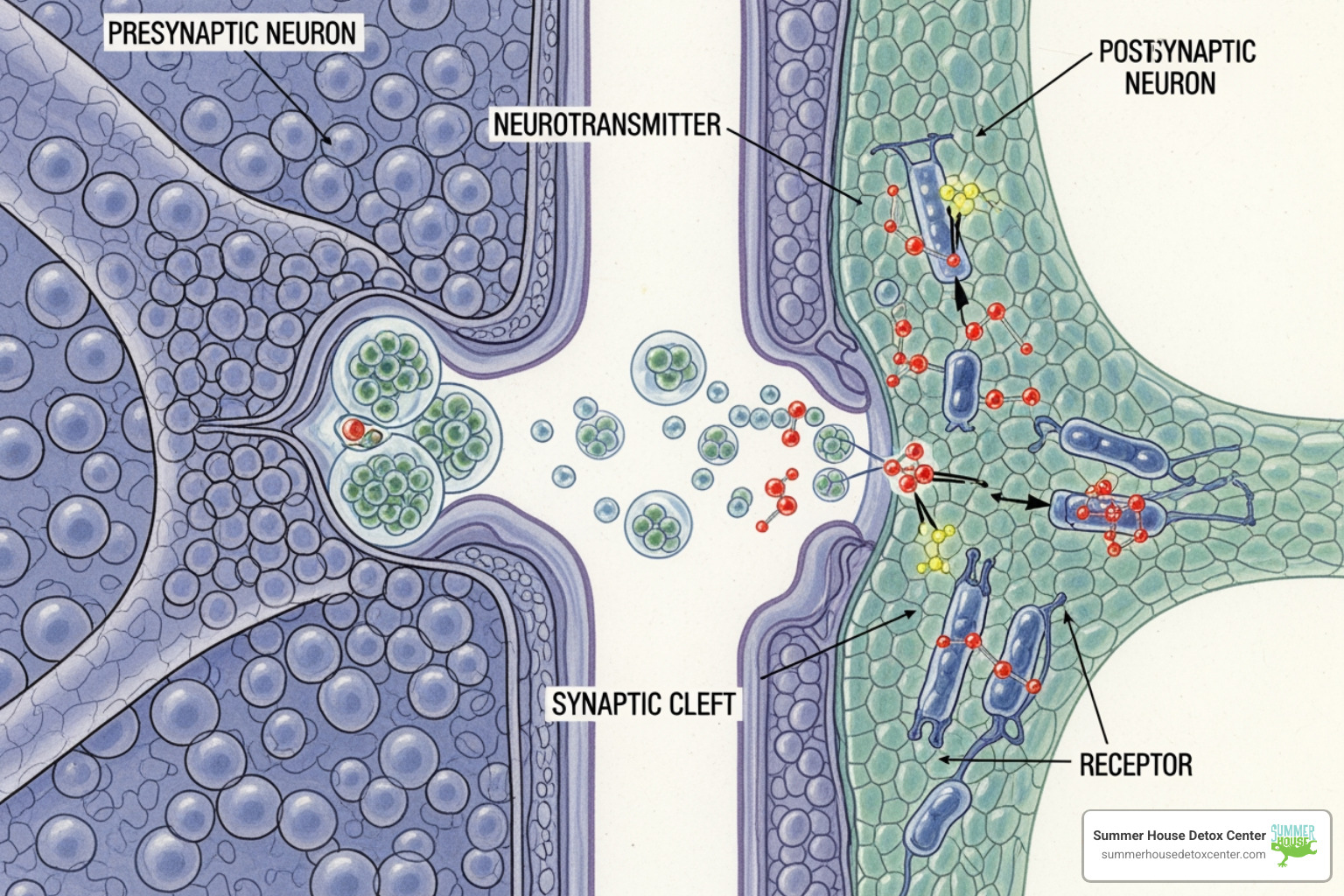
MAT works by rebalancing the brain’s chemical messengers, called neurotransmitters. For example, substances of abuse flood the brain with dopamine, creating a powerful sense of pleasure. Over time, this alters the brain’s natural dopamine system, leading to cravings and dependence. MAT medications help normalize these systems, reducing the compulsive drive to use substances.
For a deeper dive into this foundational approach, you can explore our page on Understanding Medication-Assisted Treatment.
How Medications in MAT Work
The medications used in addiction medication therapy work on the brain’s neurotransmitter systems in different ways:
- Agonists: These medications activate brain receptors, mimicking the abused substance’s effects but in a milder, more controlled way. This reduces withdrawal and cravings without the intense “high.” Methadone is an example.
- Partial Agonists: These activate receptors less than full agonists. They prevent withdrawal and cravings without a full euphoric effect, making misuse less likely. Buprenorphine is a partial agonist.
- Antagonists: These block receptors, preventing the abused substance from producing its euphoric effects. This helps break the cycle of use. Naltrexone is an antagonist with no misuse potential.
- Mixed Agonist-Antagonists: These have a dual action, stimulating some receptors while blocking others. This provides a complex way to manage cravings and block unwanted effects while the medication is active.
By carefully selecting the right medication, we can help individuals stabilize their brain chemistry, diminish cravings, and reduce the likelihood of relapse, providing a strong foundation for their recovery journey.
Diagnosing a Substance Use Disorder (SUD)
An accurate diagnosis of a Substance Use Disorder (SUD) is essential before starting addiction medication therapy. At Summer House Detox Center and other reputable Florida facilities, this begins with a thorough evaluation by a psychiatrist, psychologist, or licensed drug and alcohol counselor.
Mental health professionals use criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to diagnose SUDs. The diagnosis is based on a cluster of cognitive, behavioral, and physiological symptoms indicating continued use despite significant problems. The severity of symptoms helps tailor the treatment plan.
Lab tests can monitor drug use but don’t diagnose the disorder itself. The diagnosis relies on a comprehensive clinical interview and patient history. Honesty about substance use is crucial for creating a personalized care plan. For those in Miami or elsewhere in Florida, finding a local, licensed professional for this assessment is the critical first step.
FDA-Approved Medications for Substance Use Disorders
The medications used in addiction medication therapy are rigorously tested and approved by the U.S. Food and Drug Administration (FDA) for safety and effectiveness. This approval is a cornerstone of evidence-based treatment.
These medications are not “trading one drug for another.” They work to normalize brain function, reduce cravings, and prevent withdrawal, allowing individuals to engage more effectively in counseling. Treatment is clinically driven and customized to each person’s needs, contributing to a “whole-patient” approach.
For more information on the range of FDA-approved options, SAMHSA provides valuable resources, including their page on Medications for Substance Use Disorders – SAMHSA.

Medications for Opioid Use Disorder (OUD)
Medications for Opioid Use Disorder (MOUD) are highly effective at helping individuals reduce illicit opioid use, stay in treatment, and significantly lower the risk of overdose. MOUD can normalize brain chemistry, block the euphoric effects of opioids, relieve cravings, and restore normal body functions.
The three primary FDA-approved medications for OUD are:
- Methadone: A long-acting opioid agonist, methadone is dispensed daily in licensed opioid treatment programs (OTPs) across Florida. It prevents withdrawal, reduces cravings, and blocks the euphoric effects of other opioids. It has been a highly researched and effective treatment for over 50 years. Learn more on our page, Which Medications Are Used in Opiate Detox?.
- Buprenorphine: A partial opioid agonist, buprenorphine produces milder effects than methadone. It can be prescribed in a physician’s office, increasing access to treatment. It reduces cravings and withdrawal and is often combined with naloxone (e.g., Suboxone) to deter misuse. See our articles, Methadone vs. Suboxone: How Do They Differ? and Does Suboxone Help With Opiate Withdrawal Symptoms?.
- Naltrexone: A non-addictive opioid antagonist, naltrexone blocks opioid receptors, preventing any opioid from having an effect. Available as a daily pill or monthly injection (Vivitrol), it’s used after detox to prevent relapse and reduce cravings.
While less common, Lofexidine is also an FDA-approved non-opioid medication that helps reduce opioid withdrawal symptoms.
Here’s a quick comparison of the main OUD medications:
| Medication | Mechanism of Action | Administration | Key Benefits |
|---|---|---|---|
| Methadone | Full Opioid Agonist | Daily liquid (OTP clinics) | Reduces cravings & withdrawal, blocks euphoric effects of other opioids, long history of effectiveness. |
| Buprenorphine | Partial Opioid Agonist | Sublingual film/tablet, injection | Reduces cravings & withdrawal, milder opioid effects, can be prescribed in doctor’s office, often combined with naloxone to deter misuse. |
| Naltrexone | Opioid Antagonist | Daily pill, monthly injection | Blocks all opioid effects, non-addictive, no misuse potential, used to prevent relapse after detox, can also be used for AUD. |
Medications for Alcohol Use Disorder (AUD)
Addiction medication therapy is also incredibly effective for Alcohol Use Disorder (AUD). Combined with counseling, medications for AUD (MAUD) can reduce drinking, manage cravings, and improve outcomes.
The main FDA-approved medications for AUD include:
- Naltrexone: Also used for OUD, naltrexone blocks the brain’s opioid receptors involved in the rewarding effects of alcohol. This reduces cravings and the pleasure from drinking, making it easier to cut back or abstain. It comes as a daily pill or monthly injection (Vivitrol).
- Acamprosate: This medication helps restore brain chemistry disrupted by chronic drinking. It reduces the emotional and physical distress of prolonged abstinence, helping maintain sobriety. It’s usually started after detox is complete.
- Disulfiram: This medication creates an unpleasant physical reaction (nausea, headache, flushing) if alcohol is consumed. This immediate, undesirable consequence acts as a strong deterrent to drinking.
These medications are powerful tools for managing AUD. To learn more, visit our page on What Type of Medications Are Used in Alcohol Treatment?.
Medications for Nicotine Cessation
While our focus at Summer House is on alcohol and opioid detox, it’s worth noting that addiction medication therapy also extends to nicotine addiction. Medications can significantly improve the chances of quitting.
FDA-approved options include:
- Nicotine Replacement Therapies (NRT): Patches, gums, and lozenges deliver controlled nicotine doses to reduce cravings and withdrawal.
- Bupropion (Zyban): An antidepressant that reduces nicotine cravings and withdrawal symptoms.
- Varenicline (Chantix): Targets nicotine receptors to reduce the pleasure of smoking and ease withdrawal.
These medications, combined with behavioral support, are effective for those trying to quit nicotine products.
The Power of Integration: Why Addiction Medication Therapy Includes Counseling
It’s vital to understand that addiction medication therapy is more than just medication. Effective treatment must address the “whole person.” While medications stabilize brain chemistry, they are not a “magic pill.” Lasting recovery requires addressing the underlying psychological, social, and environmental factors contributing to addiction.
This is why counseling and behavioral therapies are indispensable. As NIDA emphasizes, effective treatment attends to multiple needs, not just substance use. You can learn more about this integrated approach on our page, Combining Medical and Natural Therapies for Recovery, and in NIDA’s research on Treatment and Recovery | National Institute on Drug Abuse (NIDA).
The Role of Behavioral Therapies in Addiction Medication Therapy
Behavioral therapies are the cornerstone of addressing the psychological aspects of addiction, teaching crucial skills for maintaining sobriety.
- Cognitive Behavioral Therapy (CBT): Helps patients identify and change problematic thinking and behaviors related to substance use, teaching coping strategies for triggers and cravings.
- Contingency Management (CM): Uses positive reinforcement (e.g., vouchers) to encourage sobriety and treatment attendance.
- Motivational Improvement Therapy (MET): Helps resolve ambivalence about recovery and strengthens a person’s motivation to change.
- Family Therapy: Involves family members to improve communication, address relational issues, and build a supportive home environment, which is especially critical for adolescents.
These therapies help individuals develop coping skills, identify triggers, and build a strong support network. For a comprehensive guide, refer to NIDA’s Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition).
Benefits of a Comprehensive Addiction Medication Therapy Program
Combining medication with behavioral therapy leads to significantly better outcomes. A comprehensive addiction medication therapy program offers many benefits:
- Improved Survival Rates: Medications for OUD are shown to improve patient survival by reducing overdose risk.
- Increased Treatment Retention: Patients in MAT are more likely to stay in treatment, a key predictor of long-term success.
- Decreased Illicit Substance Use: MAT significantly decreases illicit opiate use and related criminal involvement.
- Increased Employment: Improved stability and health increase patients’ ability to gain and maintain employment.
- Improved Birth Outcomes: For pregnant women with SUDs, MAT can improve outcomes for both mother and child.
- Reduced Risk of HIV/Hepatitis C: By decreasing illicit drug use and risky behaviors, MAT lowers the risk of contracting infectious diseases.
Our page on Medications and Recovery further details how these combined approaches lead to healthier, more stable lives.
Accessing MAT in Florida: Your Path to Treatment
The duration of an addiction medication therapy journey varies for each person. There’s no one-size-fits-all timeline. Factors like addiction severity, clinician recommendations, and patient goals all play a role. Some may use medication short-term, while others benefit from long-term use to maintain stability. Treatment plans are flexible and adjusted as your needs change.
Cost is a common concern. The good news is most health insurance plans cover MAT, thanks to the Mental Health Parity and Addiction Equity Act (MHPAEA). This law requires insurers to cover substance use disorder treatment at the same level as other medical care. If your plan covers medical care, it should also cover your addiction medication therapy.
Preparing for your first appointment is a crucial step. Be open and honest with your provider about your substance use history, mental health, and recovery goals. It’s also helpful to list your questions and any current medications or supplements.
How to Find MAT Services in Miami and Florida
Finding the right MAT services in our local community, whether in Miami or across Florida, is easier than you might think. Several excellent resources are available to help you locate providers:
- SAMHSA Behavioral Health Treatment Services Locator: This confidential tool from the Substance Abuse and Mental Health Services Administration (SAMHSA) can help you find facilities in Florida. Visit SAMHSA Behavioral Health Treatment Services Locator.
- Florida DCF Treatment for Substance Abuse: The Florida Department of Children and Families also provides resources on treatment options available throughout the state. Check their website at Florida DCF Treatment for Substance Abuse.
- Buprenorphine Provider Locators: To find providers who can prescribe buprenorphine for OUD, SAMHSA offers a dedicated locator at Buprenorphine Providers Locator (SAMHSA).
- Summer House Detox Center: Here in Miami, we offer comprehensive Medication-Assisted Treatment as part of our detox services. Learn more about our programs at Summer House Detox Center Medication-Assisted Treatment.
When you’re ready, these resources can connect you with compassionate, evidence-based care in our community.
Insurance and Paying for Treatment
Navigating insurance can be complicated, but we can help. As mentioned, the Mental Health Parity and Addiction Equity Act (MHPAEA) ensures most plans cover addiction medication therapy. However, specific details like deductibles, co-payments, and network status vary by plan.
We recommend contacting your insurance provider to verify your benefits. Our team at Summer House can also assist with insurance verification to simplify the process.
For those without insurance, Florida has state-funded programs. The HHS offers guidance on Mental Health and Addiction Insurance Help (HHS). Our admissions team can also discuss payment options to make treatment accessible.
Frequently Asked Questions About MAT and Recovery
We often hear common questions about addiction medication therapy and the nature of recovery. Let’s address some of these directly.
Can addiction be cured, or is it a manageable chronic condition?
The scientific consensus is that addiction is a chronic, manageable condition, similar to diabetes or heart disease. It cannot be “cured” in the sense that it disappears forever. However, it can be successfully managed, allowing individuals to achieve sustained remission and lead fulfilling lives. Addiction involves long-lasting brain changes, and while treatment helps regain control, vulnerability to relapse can persist. The focus is on long-term management and relapse prevention, not eradication.
Does relapse mean that addiction treatment has failed?
Absolutely not. Relapse is a common part of recovery for any chronic condition, including addiction, and it is not a sign of failure. Relapse rates for addiction are similar to those for other chronic illnesses like asthma or hypertension. We view relapse as a sign that the treatment plan needs adjustment—perhaps a change in medication, therapy, or support level. The goal is to learn from the relapse, identify triggers, and strengthen coping skills. Reducing the stigma around relapse encourages people to seek help immediately instead of feeling shame.
Are there specific treatment considerations for adolescents?
Yes, treating adolescents requires a specialized approach because their brains are still developing, particularly in areas of decision-making and self-control. This makes them more vulnerable to substances and affects how they respond to treatment. Key considerations for adolescent addiction medication therapy and treatment include:
- Developmentally Appropriate Programs: Treatment must be custom to their specific age, maturity, and unique challenges.
- Importance of Family Involvement: Behavioral therapies involving family are often highly beneficial for improving communication and creating a supportive home environment.
- Co-occurring Mental Health Disorders: Adolescents with SUDs often have co-occurring issues like ADHD, depression, or anxiety that should be treated concurrently.
- Medication Options: For opioid use disorder, buprenorphine is approved for adolescents aged 16 and over.
Understanding these unique needs is essential for providing effective care. NIDA’s Principles of Adolescent Substance Use Disorder Treatment: A Research-Based Guide offers more insights into these specialized approaches.
Begin Your Recovery Journey in Miami
We understand that taking the first step toward recovery can feel overwhelming, but we want you to know that addiction is a treatable disease, and recovery is absolutely possible. Here at Summer House Detox Center in Miami, we believe in a compassionate, comprehensive approach that addresses your unique needs. We are dedicated to reducing the stigma surrounding addiction and its treatment, creating a supportive environment where you can heal with dignity.
Our medically supervised detox programs, including addiction medication therapy, are designed for your comfort and safety. Our experienced team, some of whom are in recovery themselves, provides personalized care every step of the way. If you’re looking for a path to recovery in Florida, we invite you to explore our Medication-Assisted Treatment services and find how we can help you regain control of your life. Your journey to a healthier, happier future starts here.
